Can Electrical Stimulation Treat Chronic Wounds?
Introduction
The short answer to the question is yes it can. Although there is a lot of research literature on the topic, it is reasonable to suggest that the application of electrical stimulation to help resolve chronic wounds is not that well understood or widely practised yet. There are a variety of different approaches and there is perhaps no optimal approach that has yet been identified. As a consequence, the evidence supporting electrical stimulation for wound healing is always muted due to the variety of protocols that have been used. Perhaps the approach with the longest use is High Voltage Pulsed Current (HVPC) which dates back to the 1940s. So called low-intensity pulsed current (LIPC) has also been used. LIPC delivers short, low-voltage electrical pulses to the wound. These pulses help to increase blood flow and the production of growth factors, which are proteins that promote wound healing. In this article, we will take a look at the nature of wounds, the rationale behind electrical stimulation for wound healing and look at some of the approaches that have been taken.
The problem of chronic wounds
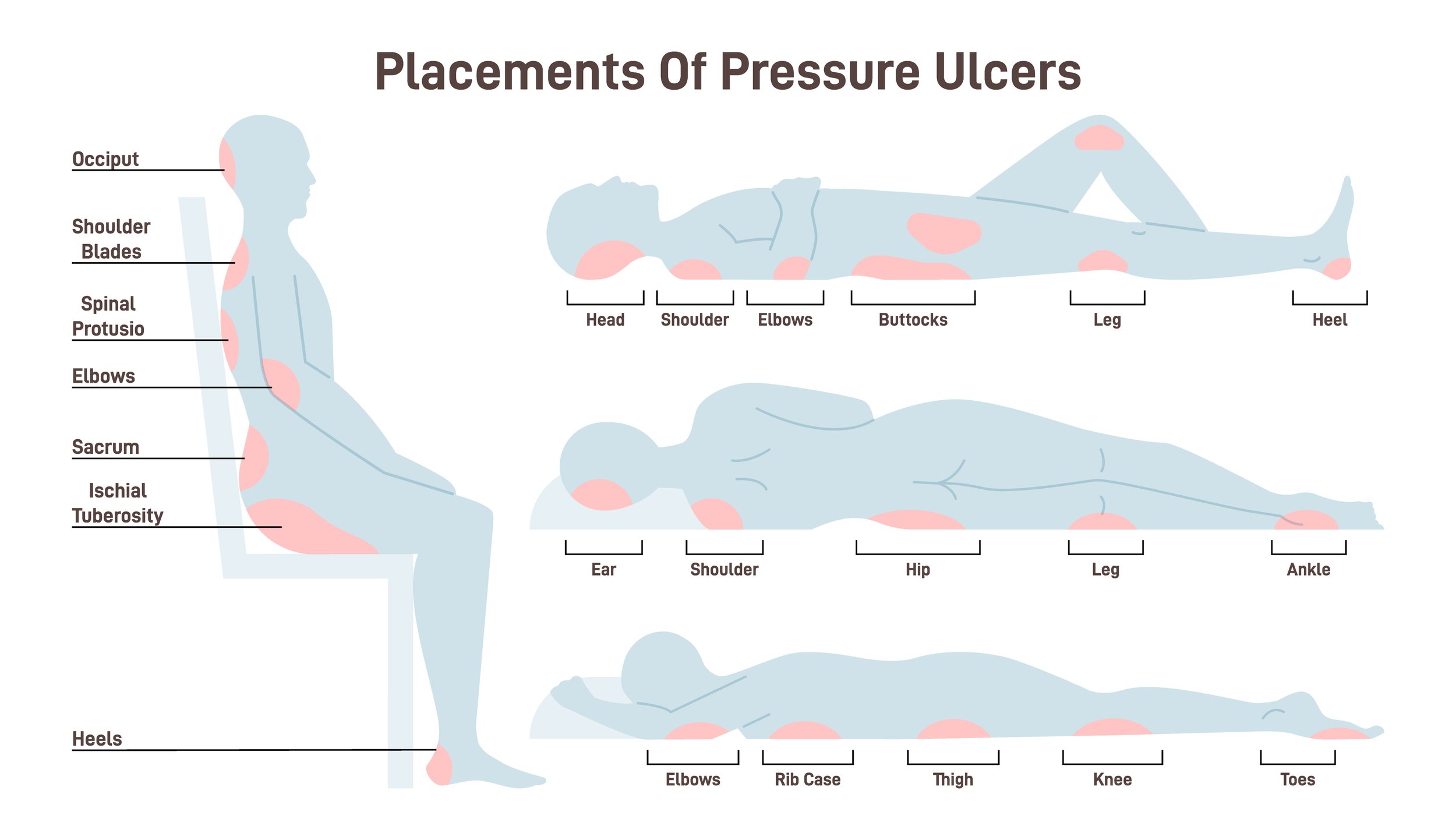
You could say that a great deal of Anatomical Concepts business is focused on the type of wounds described as pressure ulcers. Our PRAFO range of ankle-foot orthoses is considered the market-leading product range for heel pressure ulcer prevention and treatment. Pressure ulcers, as we frequently say, are much better prevented if possible as the consequences of tissue breakdown are costly from many points of view - human and financial. The image adjacent highlights areas where pressure ulcers are most likely to occur; being regions where bony prominencies are close to the body surface. Vulnerable persons may be relatively immobile and have a range of additional risk factors.
Once wounds occur, there is a heightened risk of infection and often tissue at a prior wound site can remain fragile even when healed due to the changes in tissue structure. We have discussed the causes and challenges of wounds in several previous articles.
The general problem of wound management is not a new one and sadly it is a growing problem with current NHS expenditures for treatment amounting to more than ᆪ8 billion per year with a 71% increase in prevalence from 2012/2013 to 2017/2018. (Guest et al, 2020). According to a report by Posnett et al (2008) more than 400,000 people in the UK have chronic wounds with venous leg ulcers being the most common.
Of course, there is much attention on "lotions and potions" for wound healing but, especially with pressure ulcers, the real remedy is not what you "put on" the ulcer but what you take off. Many medical factors increase the risk of pressure ulcers and wounds in general so the specific mechanical and medical causes of wounds need careful consideration in each case. There is no "silver bullet" - no single approach suitable for all cases.
Treatment of wounds should involve dealing with both mechanical and medical factors. Relieving pressure and shear is an essential part of treatment. In addition, there are many varieties of wound dressings and "skin substitutes" that are frequently used but generally lack evidence of effectiveness; and chronic wounds, in particular, don't tend to respond to these measures. Skin grafting may be offered for chronic wounds but this is far from being an easy solution.
If electrical stimulation can be effective this would be a nice solution as it is generally safe, non-invasive and relatively low cost once any capital equipment has been acquired.
What's a chronic wound?
A chronic wound has not responded to the usual therapies within a reasonable time frame and this can be due to many factors. These include inadequate vascularity, infection, medications that impair healing (such as steroids), immunological disorders, or secondary to radiation therapy. A chronic wound is a description of a "state" rather than a specific cause and these may arise due to a variety of pathophysiologies such as pressure ulcers, diabetic foot disease, and arterial or venous ulcers.
Chronic wounds therefore often have multiple causes and the challenge for clinicians in resolving them is to apply a multi-factorial approach to diagnosis first and then treatment. In addition to the traditional treatments of pressure offloading, wound dressings and infection control, electrical stimulation has become an increasingly used therapy.
The rationale for using electrical stimulation
Electrical stimulation involves the application of small doses of electricity directly onto the skin near the wound. The first question you might reasonably ask is
"Who decided this was a good idea?"
The answer depends on how far you want to go back. Electricity has been applied to the human body for therapeutic purposes since the 18th Century. Unfortunately, this journey has been tainted by quacks and charlatans from time to time which has probably contributed to the relative ignorance of today's clinicians about what works and what doesn't. We will leave the broader discussion of electrotherapy in history to another day and restrict our discussion to that relevant to wound healing.
Personally speaking, I first worked with electrical stimulation for wound healing back in the late 1970s and have noted that it has moved in and out of fashion ever since. Part of the challenge in researching the evidence for electrical stimulation is that there are so many defining parameters. Electrical stimulation waveforms in use can vary a great deal in their
pulse shapes
whether bipolar or unipolar
pulse widths
frequency
whether delivered continuously or in bursts
current/voltage levels
So often when we review the literature, the parameters used in a study are not defined so it becomes hard to conclude on "the best" settings. Electrical stimulation is not "one thing" - the specific stimulation parameters used are important and in practice, one or more parameters will need to be tailored to the individual situation. There are likely no optimal settings for all situations.
The skin battery
Much of the rationale for using electrical stimulation to treat wounds stems from the fact that the skin and deeper tissues naturally carry an electrical charge which is essential to tissue health. This is sometimes referred to as a skin battery or transepithelial potential.
The transepithelial potential is a small electrical charge (approximately 23 milliVolts) that naturally exists on the surface of the skin relative to the deeper tissues. The deeper tissues have a positive polarity relative to the skin surface. This electrical potential plays an important role in maintaining tissue health, controlling electrolyte transport across cell membranes, and regulating cellular activities such as wound healing. If a wound occurs this charge potential is disrupted. You could say that the skin battery is "short-circuited."
You could say that the rationale for using electrical stimulation is to restore the integrity of the skin battery.
The architecture of skin
The biological makeup of skin and its physiological state determine its electrical properties so it is worthwhile to consider some aspects of its structure which are relevant to electrical stimulation.
The normal makeup of these tissues affects how easily electrical energy can penetrate.
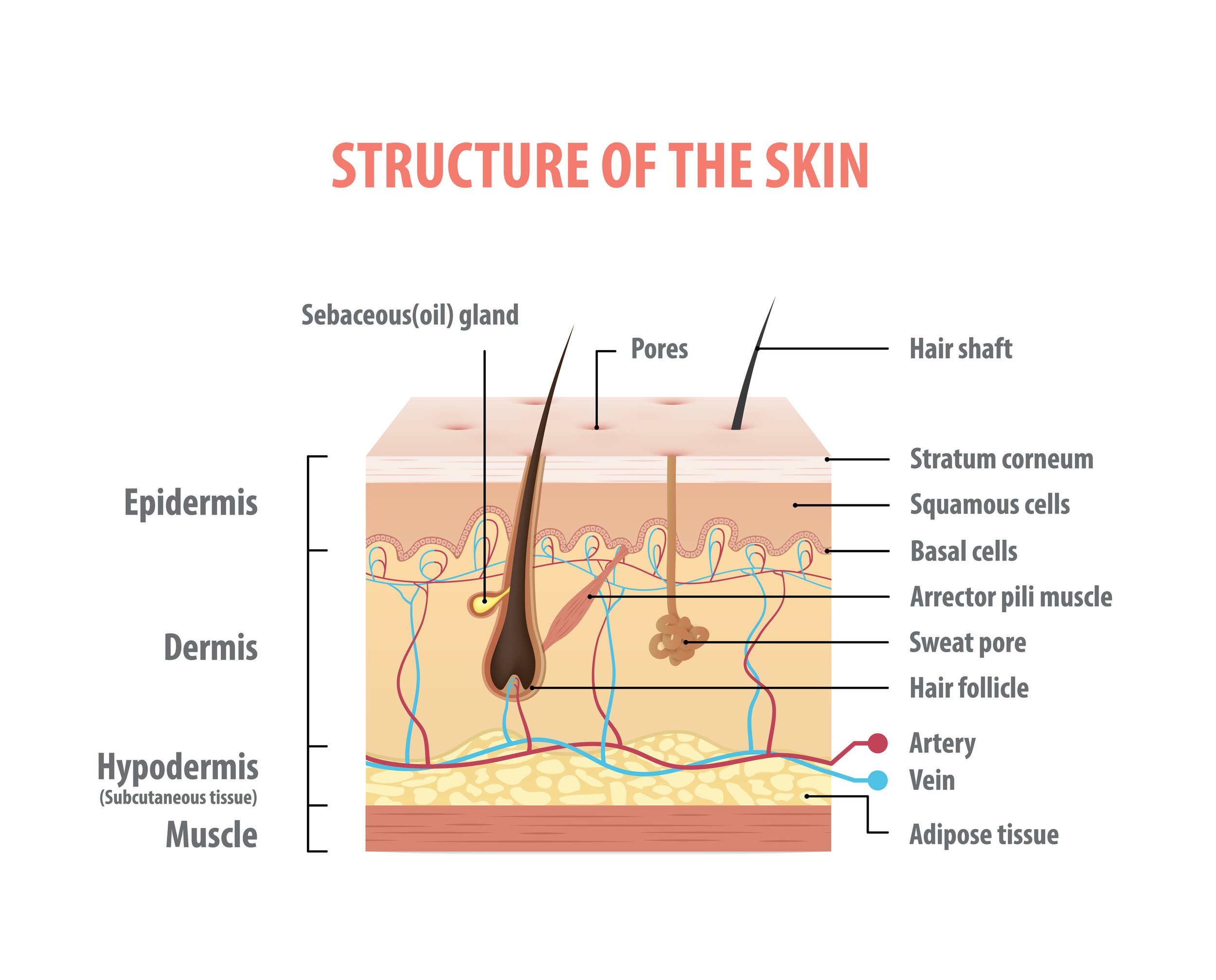
Examined microscopically, the skin is found to have two distinct layers, the dermis and epidermis.
The dermis and epidermis together constitute the skin. The epidermis is punctured by sweat gland ducts and hair follicles. Beneath the skin is the subcutis, also referred to as the superficial fascia or simply subcutaneous tissue. Blood vessels, lymph vessels and nerves infiltrate the subcutis and dermis but not the epidermis.
There are other fundamental differences between the dermis and epidermis. The dermis is well hydrated and consists of a matrix of collagen and elastin fibres embedded in a 'ground substance' rich in proteoglycans and hyaluronic acid. Fibroblasts are the predominant cells in this layer.
The high degree of hydration makes the dermis electrically conductive. The epidermis is less hydrated and consists of a matrix of keratin fibres. The cells present in this layer are predominantly keratinocytes which receive nutrients from capillaries in the underlying dermis.
The basal layer of the epidermis is metabolically very active, with the cells regularly undergoing mitosis. Keratinocytes form and pushed upwards from this layer, synthesise keratin and store it within the cytoplasm.
In their life cycle, the keratinocytes move towards the skin surface, becoming less metabolically active as diffusion limits the rate of nutrient supply. Near the surface the cells die and shrivel, turning into little sacs of (mostly) keratin. The dead cells form a scaly shell called the stratum corneum.
The stratum corneum is the dehydrated remains of keratinocytes packaged full of keratin. Formation in the basal layer to desquamation takes the keratinocyte approximately 40 days. The balance between desquamation and mitosis in the basal layer keeps the thickness of the epidermis constant.
The stratum corneum is a dry, insulating, but very thin shell which separates and isolates the highly hydrated soft tissues of the human body from the drier and far more changeable external environment. If the stratum corneum is removed, the body loses water and if too great an area of the stratum corneum is lost or damaged, the resulting water loss can be fatal. As noted above, the fibrous protein, keratin forms the bulk of this dead, insulating layer which is so essential for water homeostasis.
From the point of view of electrical stimulation penetrating the skin, the presence of the stratum corneum is significant because it acts as an electrical insulator. When we use electrical stimulation and wish to activate a nerve, (a common application) we want the energy to penetrate deep into the tissues so knowledge of the skin and tissues' electrical properties is very important to the design of the stimulator. The type of waveform we must use is affected by the skin and tissue's electrical properties also. We will come back to this topic shortly.
Clinical practice guidelines
As you would expect, there are several clinical practice guidelines available for the prevention and treatment of ulcers. This one shown here (Consortium for Spinal Cord Medicine, 2020) is specific to pressure ulcers with spinal cord injury.
It does mention electrical stimulation to promote wound closure (p43). and mentions High Voltage Pulsed Current Electrical Stimulation but does not define the specifics of this form of stimulation.
In a Cochrane review, by Arora M et al (2020), the authors examined published and unpublished studies (n=20) with around 900 participants in a meta-analysis to determine the effects (benefits and harms) of electrical stimulation for treating pressure ulcers.
The authors state that electrical stimulation probably increases the proportion of pressure ulcers healed compared with no electrical stimulation. In conclusion, the authors state that electrical stimulation is widely used for the treatment of pressure ulcers. However, they say it is not clear whether it is effective.
High Voltage Pulsed Current (HVPC)
High Voltage Pulsed Current (HVPC) has been used in therapy since the 1940s, and you will find lots of references to its use in wound healing, pain relief and oedema reduction. As is still common in electrical stimulation circles, some authors use different terms to describe HVPC - such as "twin peak monophasic" - which is a cause of confusion.
This waveform is in effect a monophasic pulsed current. Pulses are delivered as a pair of very short-duration pulses of high voltage in the range 150 Volts and up to 500 Volts. Typically these pulses are of very short duration and with a sharp peak rather than rectangular. This means that the energy in them is typically quite low. The effective current is in the microamp range and the polarity means that only a small current flow will penetrate the skin. This could in effect be described as a microcurrent therapy. Devices using this approach may allow some control of the interval between pulse pairs and the time interval between these pairs.
There are many trials of HVPC for wound healing and there is little doubt that HVPC can influence wound healing in the clinical environment. There are several other forms of electrical stimulation which have also been demonstrated and what is lacking is a comparative trial which directly compares different forms of stimulation with a common research method.
In my experience, I have found bipolar, rectangular pulses to be effective although I have never tried to compare these approaches. The technology has advanced a great deal and I don't know how much the use of HVPC has been simply a product of the technical limitations of the 1940s. Certainly, I have no belief that HVPC is the only waveform that can be effective.
Practical implementation
As a starting point, I would recommend the following which we achieve with either a RehaStim device, an Edition 5 or a RISE stimulator. With a RehaStim device, we would typically use large adhesive electrodes and if using the Edition 5 or RISE stimulator we would use wet sponge and carbon rubber electrodes. Electrodes would be adjacent to, but never over a wound.
We would try bipolar rectangular pulses with a pulse width of 250 microseconds, a frequency of 40 Hz and delivered in bursts of 4 seconds on and 4 seconds off. The current level should be just sufficient to produce a noticeable contraction. In the case of flaccid paralysis, the pulse width and frequency will need to be lower and we would use the Edition 5 or RISE units
Delivered for 1 hour per day, 7 days per week. A great deal of patience and time will generally be required and progress should be monitored closely.
In addition, any wound dressings containing metal ions (eg silver) should be removed from the area. Avoid stimulating directly over metal implants or other implanted medical devices. Avoid electrical stimulation if infection is present (although some research suggests that electrical stimulation can have an anti-bacterial effect.
We have written previously about protocols to use when red marks (pre-wound) are apparent
https://www.anatomicalconcepts.com/articles/electrotherapy-and-wound-healing-part-1
https://www.anatomicalconcepts.com/articles/electrotherapy-and-wound-healing-part-2
Conclusion
Pressure ulcers are a growing problem, both in terms of prevalence and cost to the NHS, and clinicians must utilise all available treatments when trying to heal these wounds. In addition to traditional wound care such as offloading pressure, infection control and use of dressings; electrical stimulation has become an increasingly used therapy to help with chronic wounds.
Although electrical stimulation is generally thought of as a positive intervention, ts use needs to be tailored to the individual patient’s needs and further research is needed in this area. The most widely reported is HVPC which dates back more than 80 years. More research is necessary to explore the most effective approaches for chronic wounds.
By considering electrical stimulation among other treatments we can make sure that the best possible care is given, both from a medical and financial point of view. This will help to ensure that patients receive the best possible treatment for their wounds, and that as many of these wounds can be healed as quickly and cost-effectively as possible. With careful individualised assessment and management, better outcomes may be achieved with fewer complications than with traditional wound care alone. In this way, a holistic approach to pressure ulcer management could be beneficial. With a better understanding of the evidence and correct application of electrical stimulation, more wounds may be able to heal faster with less cost and improved patient outcomes. Ultimately, this could result in a significant reduction of pressure ulcers globally.
References
Guest JF, Fuller GW, Vowden P (2020) Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013BMJ Open 2020;10:e045253. doi:10.1136/bmjopen-2020-045253
Posnett J, Franks PJ. (2008) The burden of chronic wounds in the UK. Nurs Times. 2008 Jan 22-28;104(3):44-5. PMID: 18293879.
Arora M, Harvey LA, Glinsky JV, Nier L, Lavrencic L, Kifley A, Cameron ID (2020). Electrical stimulation for treating pressure ulcers, Cochrane Database of Systematic Reviews, 2020. NO: 1, John Wiley & Sons, Ltd. DOI: 10.1002/14651858.CD012196.pub2, US: https://doi.org//10.1002/14651858.CD012196.pub2
Consortium for Spinal Cord Medicine - Pressure Ulcer Prevention and Treatment Following Injury: A Clinical Practice Guideline for Health-Care Providers - 2020. ISBN 0-929819-24-1
Gardner, S. E., R. A. Frantz and F. L. Schmidt (1999). "Effect of electrical stimulation on chronic wound healing: a meta-analysis." Wound Repair Regen 7(6): 495-503.
Gentzkow, G. D. and K. H. Miller (1991). "Electrical stimulation for dermal wound healing." Clin Podiatr Med Surg 8(4): 827-841.
Robinson, A. J. (2008). Electrical stimulation to augment healing of chronic wounds. Clinical Electrophysiology: Electrotherapy and Electrophysical Testing. A. J. Robinson and L. Snyder- Mackler. Philadelphia, Lippincott Williams & Wilkins: 275-299.
Disclaimer
This article is offered as general information on this topic and should not be interpreted as medical advice. Wounds are serious healthcare challenges and require comprehensive assessment and individual treatment plans.