Articles
Filter by Topic
- Adaptive Sport 1
- Artificial Intelligence 1
- Bike Labyrinth 3
- Bone density 1
- Brachial Plexus 2
- Bridging the Gap 1
- Bridging the Gap 1
- Carbonhand 4
- Cardiovascular 1
- Cauda Equina Syndrome 1
- Client Stories 4
- Cognition 1
- Company Updates 3
- Decision Making 2
- Dementia 1
- Denervation 26
- Diabetic Foot 12
- Efficiency 1
- Electrotherapy 32
- Exercise Benefits 33
- FES Cycling 19
- Fatigue 1
- Functional Electrical Stimulation (FES) 61
- Gait 2
- Goal Setting 5
- Grip 3
- Guidelines 1
- HRV 1
- Healthspan 2
- Indego 13
- Lifestyle 10
- Lower Motor Neuron 1
- Mobility 17
- Motivation 2
- NMES 2
- Nerve injury 2
- NexStride 1
- Occupational Therapy 1
- Orthotic 15
- PRAFO 28
- Pain 7
- Parkinsons 2
- Pressure Ulcers 15
- Product Updates 7
- RISE Stimulator 12
- Safety 2
- Spasticity 2
- Sponsor 1
- Standing 5
- Stim2Go 6
Article Length
- 1 minute read 3
- 10 minute read 21
- 11 minute read 4
- 12 minute read 10
- 15 minute read 13
- 18 minute read 1
- 2 minute read 4
- 24 minute read 1
- 25 minute read 1
- 26 minute read 1
- 28 minute read 1
- 3 minutes read 9
- 4 minute read 34
- 5 Minute read 15
- 6 minute read 6
- 7 minute read 17
- 8 minute read 7
- 9 minute read 3
- FES 2
- FoG 1
- Long Read 1
- PRAFO 1
- Seven Minute Read 1
- awareness 1
- carbonhand 2
- cognitive 1
- cues 1
- freezing gait 1
- freezing of gait 1
- gait 1
- neurological 1
- neuroplasticity 1
- nexstride 2
- occupational therapy 1
- occupational therapy day 1
- orthopaedics 1
- orthotic 1
- parkinson's 1
- pressure 1
- pressure relief 1
- prevention 1
- rehabilitation 2
- stroke 1
- ulcers 1
- world stroke day 1
Transcutaneous Vagus Nerve Stimulation and Transcutaneous Spinal Cord Stimulation - Parallels for Rehabilitation Practice
Two non-invasive neuromodulation technologies — transcutaneous vagus nerve stimulation (tVNS) and transcutaneous spinal cord stimulation (tSCS) — are reshaping how we think about neurological rehabilitation.
Although they target different levels of the nervous system, these modalities share a surprising number of fundamental principles. Understanding these parallels gives clinicians, patients, and carers a clearer picture of how modern neuromodulation works, what to expect from treatment, and why these technologies represent a genuine shift from compensatory to restorative rehabilitation.
This article identifies ten fundamental parallels between tVNS and tSCS, drawing on the published scientific evidence to explore what they have in common, where they differ, and what this means for clinical practice.
Electrical Stimulation After Nerve Repair Surgery: When to Start and What to Expect
Nerve repair surgery—whether nerve grafting, nerve transfer, or direct repair—offers hope for people with peripheral nerve injuries, including brachial plexus injuries. However, surgery is just the beginning of the recovery journey. After the surgeon has reconnected or rerouted nerves, there's a waiting period while regenerating nerve fibres grow toward their target muscles. This process is slow, measured in months rather than weeks.
During this waiting period, a critical question arises: what happens to the muscles? Without nerve signals, they begin to atrophy and deteriorate. If the muscle degenerates too severely before reinnervation occurs, even successful nerve regeneration may not restore function—the nerve reconnects, but finds a muscle no longer capable of responding.
This is where electrical stimulation plays a crucial role. By keeping muscles viable during the reinnervation window, stimulation can significantly improve the chances of functional recovery. In this article, I'll explain how nerve regeneration works, when to consider electrical stimulation, and what to expect throughout the process.
Why structure beats willpower in neurological rehabilitation
If motivation were enough, rehabilitation adherence (sticking to the effort of training to recover) would not decline so predictably. But it does. Across conditions, across populations, the pattern is the same: strong engagement in the early weeks, followed by a steady fade. Not because people stop wanting to recover — but because motivation, by its nature, is temporary. It is a mood, not a method.
After decades of working in this field, I can tell you that the people who sustain their efforts over months and years are rarely the most motivated. They are the most structured. They have built something that works regardless of how they feel on any given morning — when they are tired, in pain, frustrated by slow progress, and wondering whether any of this is actually working.
To achieve significant functional gains and take advantage of neuroplasticity, it takes sustained, high-quality repetitions. Without structure, success will be elusive.
Cauda Equina Syndrome and Denervated Muscle: Your Options for Long-Term Health
Cauda equina syndrome (CES) is one of the most challenging situations in spinal cord injury rehabilitation. Unlike injuries higher in the spine, CES directly damages the lower motor neurons—the nerve cells that connect to and control the leg muscles. This results in the muscles becoming denervated, losing their nerve supply completely.
For many years, people with CES were told little could be done about the muscle wasting that occurs. The common belief was that denervated muscles would inevitably weaken, and electrical stimulation—which is effective for higher spinal injuries—simply wouldn't help. That perspective has shifted.
Research over the past twenty years shows that denervated muscles can be preserved and even improved with appropriate electrical stimulation—however, it requires a different approach from standard rehabilitation methods. In this article, I will explain what happens to muscles after cauda equina syndrome, why conventional methods often fail, and what options are available for maintaining long-term muscle and tissue health.
Why Pillows Fail: The Biomechanics of Heel Suspension
The pillow remains perhaps the most commonly used heel elevation method in hospitals worldwide. I guess this is because they are readily available, cost nothing beyond what's already supplied for patient comfort, and require no special equipment or training. They are also inadequate for heel protection and can compromise continuity of care.
The evidence is now clear: an Australian multi-centre ICU trial found that purpose-designed heel offloading devices achieved a 0.4% pressure injury incidence, compared to 8.4% with standard care, which typically means pillows and repositioning [1]. That's a twenty-fold difference. Translated into practical terms: for every 1,000 patients, 79 fewer will develop heel pressure injuries when proper offloading devices are used instead of pillows.
This isn't a criticism of clinical staff who use pillows—they're working with what's available and following long-established practice. It's an observation about biomechanics: what a pillow can and cannot achieve when the goal is heel offloading.
Understanding why pillows often fail points toward what effective heel protection actually requires.
Is the Autonomic Nervous System Ever Truly "In Balance"?
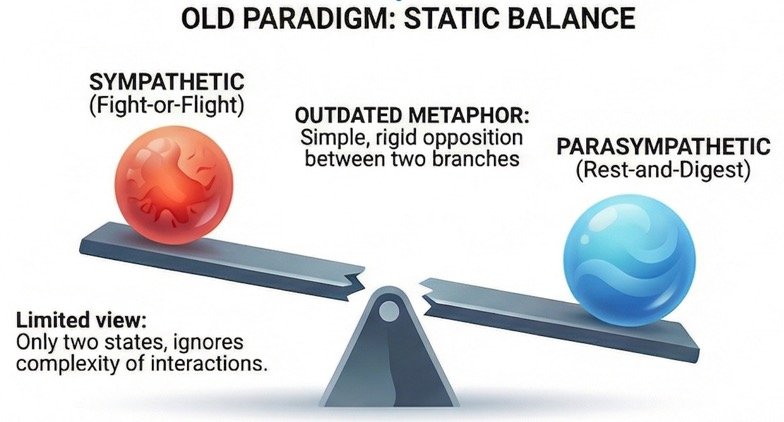
If you have been reading about the autonomic nervous system — perhaps because you live with a spinal cord injury, or you work with people who do — you will almost certainly have encountered the idea of "autonomic balance." The image is seductive: sympathetic on one side, parasympathetic on the other, and health is achieved when the two sit neatly level, like a set of scales in equilibrium.
It is a useful teaching shorthand. It is also, as modern physiology has demonstrated over the past three decades, an oversimplification that can actually mislead both clinicians and patients.
The fundamental question is this: does the autonomic nervous system ever truly achieve "balance" — and if not, what should we be aiming for instead? The answer has direct implications for how we think about autonomic dysfunction after spinal cord injury and for emerging interventions such as transcutaneous vagus nerve stimulation (tVNS) that aim to improve autonomic regulation.