Lower Motor Neuron Lesion versus Upper Motor Lesion
Introduction
In physical rehabilitation, it is often the case that intensive effort is applied to exploit the natural ability of the body to adapt to the consequences of injury. This property, known as neuroplasticity is not yet fully understood but it at least represents hope that some functional recovery is possible in many cases. In many cases there will remain a functional deficit and ultimately we find ways to compensate for function that cannot be recovered.
The nervous system is a very complex, adaptable structure, that can be disrupted by illness or injury. Rehabilitation strategies to apply in a particular case obviously depend on the nature and extent of injury.
Clinicians might refer to an "upper motor" or "lower motor" lesion when discussing a particular case. What do these terms mean? In this article we review the meaning of these statements and the consequences for rehabilitation. Some of our electrical stimulation products relate to problems with the nervous system and may help to restore or compensate for loss of function following injury or illness. Which products are relevant to these types of lesions?
Let's start by reviewing some aspects of the nervous system. Here is a quick video introduction
The Nervous System
When your nervous system functions properly, it efficiently transmits messages between your brain and body. Despite its complexity, the nervous system governs three crucial functions:
Motor functions, which enable conscious control over muscle contractions and the movement of limbs for everyday tasks.
Sensory functions, allowing you to perceive touch and be aware of limb position even with closed eyes.
Autonomic functions, which regulate actions controlled by the brain without conscious thought. Functions like heartbeat and breathing occur automatically, though it's worth noting that we can still influence them consciously. The autonomic nervous system significantly impacts various organ systems and plays a central role in our stress responses.
The nervous system therefore coordinates our actions, reactions, and interactions with the world around us. It's the highway through which messages from the brain travel to all parts of our body and back. It allows us to sense, move and react to our environment.
Lower Motor Neuron (LMN) and Upper Motor Neuron (UMN) lesions are conditions that disrupt this critical communication pathway.
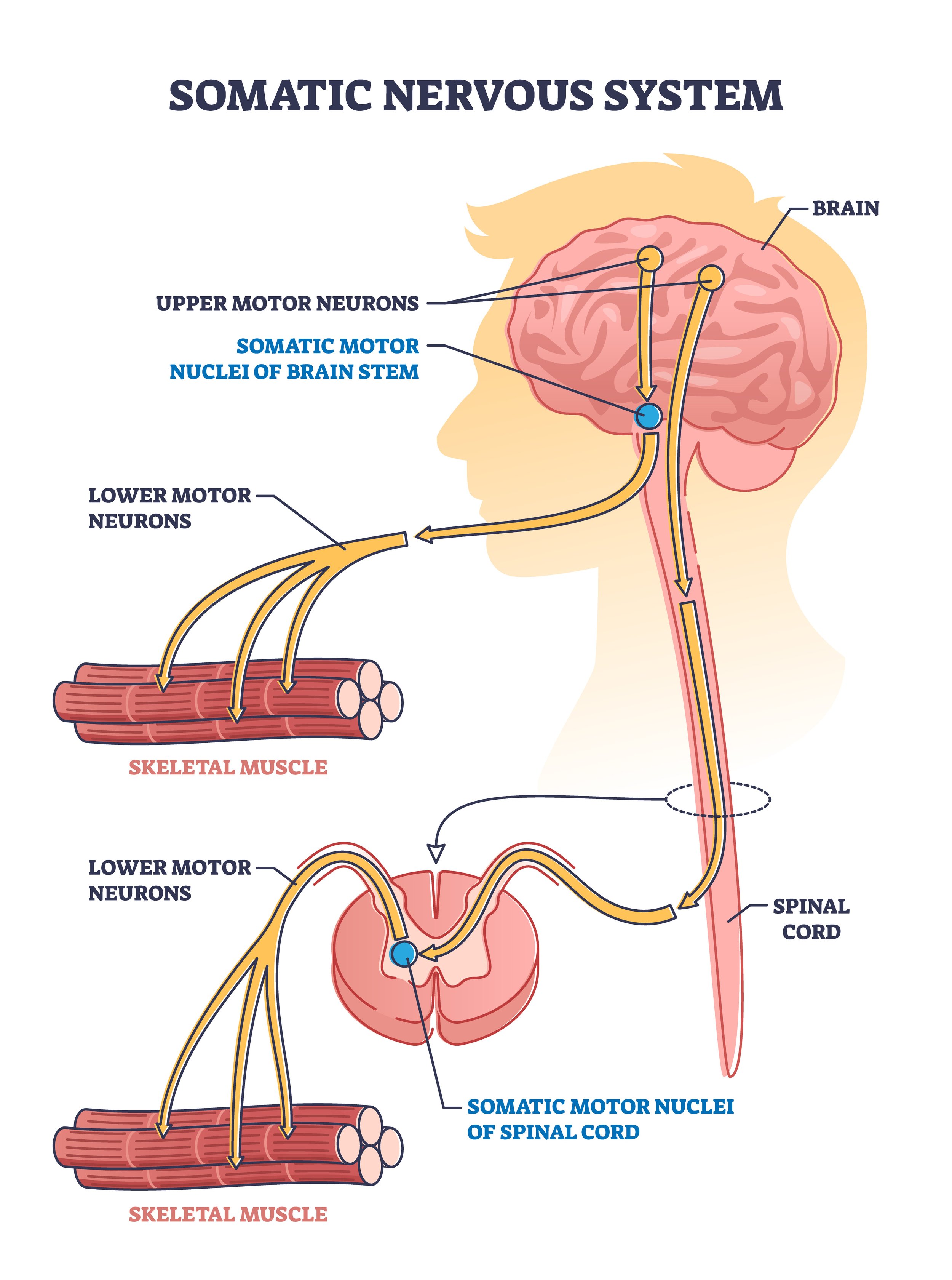
What is an Upper Motor Neuron?
An Upper Motor Neuron (UMN) is a key component of our nervous system. As the control vehicle of movement commands, it oversees the entire operation "from above".
Upper and lower motor neurons
The UMN processes the decision you make to move, sending the command down to the LMNs "below".
Therefore, if you decide to wiggle your toes, it's the UMN that initiates this action. UMNs reside within the brain's cortex, and their fibres, or axons, travel down to connect with LMNs, forming a path for our commands to follow. The interplay of UMNs and LMNs is a testament to the marvel of our bodies, a dance of neurons that allows us to interact with the world around us.
What is a Lower Motor Neuron?
A Lower Motor Neuron (LMN) is the final link in the chain; the bridge that connects our brain's commands to our muscles.
When you decide to take a step, pick up a cup, or even brush your hair, it's the LMNs who take that command and bring it to life, signalling the specific muscles involved in the action.
Consequences of injury
It is clear that anything that damages (a lesion) to either an UMN or LMN disrupts function.
Lower Motor Neuron (LMN) lesions and Upper Motor Neuron (UMN) lesions, although sharing some similar characteristics, are distinct entities each with their unique attributes and implications.
We see that LMNs, located in the spinal cord, communicate directly with muscles and govern voluntary muscle movements. An LMN lesion can lead to conditions like muscular weakness, decreased muscle tone resulting in a so-called flaccid paralysis, and reduced reflexes.
On the contrary, UMNs, found in the brain’s motor cortex, act as intermediaries in transmitting signals from the brain to the LMNs. An UMN lesion may result in symptoms like muscle stiffness, spasms, and increased muscle tone, indicative of conditions such as stroke, multiple sclerosis or some spinal cord injuries.
By delving deeper into these specific neuron lesions, we can better comprehend their impact on the body, paving the way for more effective treatments and interventions.
Conditions in which Upper Motor Neuron (UMN) Lesions can apply:
Stroke: This is one of the most common causes of UMN lesions. Strokes can cause brain damage that disrupts the normal functioning of the UMNs, leading to symptoms such as muscle weakness, spasticity, and hyperreflexia.
Multiple Sclerosis: MS is a neurodegenerative disease that causes inflammation and scarring of the myelin sheath, which can disrupt the functioning of the UMNs.
Amyotrophic Lateral Sclerosis (ALS): Also known as Lou Gehrig's disease, ALS causes degeneration of both UMNs and LMNs, leading to progressive muscle weakness and paralysis.
Cerebral Palsy: This disorder is caused by abnormal development or damage to parts of the brain that control movement, balance, and posture, which often involves UMNs.
Brain Tumors: Tumors in the brain can cause pressure or direct damage to the UMNs, leading to motor deficits.
Conditions in which Lower Motor Neuron (LMN) Lesions can apply:
Poliomyelitis: This viral infection primarily affects LMNs, leading to muscle weakness and paralysis.
Peripheral Neuropathy: This is a general term for disorders of the peripheral nerves, which can include LMNs.
Guillain-Barre Syndrome: This is an autoimmune disorder that causes inflammation of the nerves, which can affect the LMNs.
Bell's Palsy: This causes sudden weakness in the muscles of one half of the face, often due to damage to the facial nerve.
Amyotrophic Lateral Sclerosis (ALS): As noted above, ALS affects both UMNs and LMNs.
Spinal Muscular Atrophy: This is a genetic disorder that causes wasting of the skeletal muscles due to LMN loss.
Spinal Cord Injuries
At Anatomical Concepts we see may clients following a spinal cord injury.
A spinal cord injury can produce both upper and lower motor neuron injuries depending on the level and extent of the injury. In terms of motor neurons, the impact of a spinal cord injury depends on the location of the injury along the cord length:
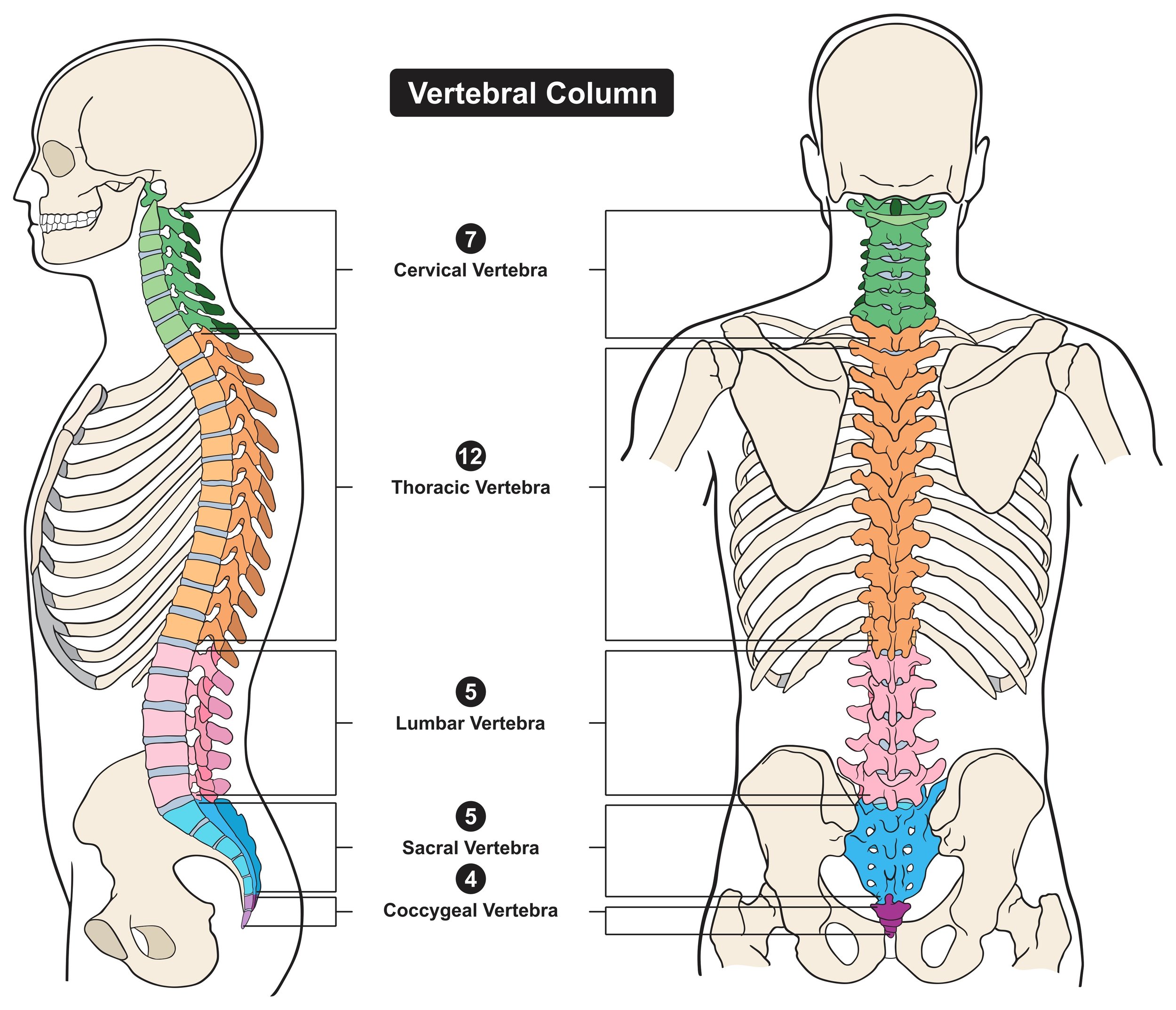
Upper Motor Neuron (UMN) Injury: If the injury occurs in the cervical or thoracic region of the spinal cord, it may affect the UMNs that originate in the brain and travel down the spinal cord to connect with LMNs at various levels below. This type of injury usually results in spastic paralysis, characterized by muscle stiffness or tightness (spasticity) and overactive reflexes (hyperreflexia).
Lower Motor Neuron (LMN) Injury: If the injury occurs at the level of the lumbar or sacral spinal cord or the the lower end of the spinal cord, it can directly affect the LMNs that exit the spinal cord at these levels. These neurons normally innervate the muscles of the lower limbs and pelvic region. LMN injuries from this cause often result in flaccid paralysis, characterised by weak, floppy muscles, reduced or absent reflexes, muscle atrophy, and sometimes muscle twitches (fasciculations).
In some cases, a person with a spinal cord injury may have both UMN and LMN symptoms. This could happen if, for example, the injury is in the cervical or thoracic regions, causing UMN symptoms in the lower body, but there is also damage to nerves as they exit the spinal cord at these levels, causing LMN symptoms in the upper body.
Therefore, the precise location and severity of the injury can influence the balance of UMN and LMN signs. Clinical evaluation and diagnostic imaging, like MRI, can help determine the extent and nature of the damage.
The bottom line is UMN and LMN lesions have different presentations and symptoms. UMN lesions are often characterized by weakness, increased muscle tone (hypertonia or spasticity), hyperreflexia, and the presence of pathological reflexes (like Babinski's sign). In contrast, LMN lesions are characterized by flaccid muscle weakness, muscle wasting (atrophy), fasciculations, and decreased or absent reflexes.
Distinguishing Between LMN and UMN Lesions
Differentiating between Upper Motor Neuron (UMN) and Lower Motor Neuron (LMN) lesions often begins with a thorough clinical examination. By assessing muscle strength, tone, bulk, and reflexes, clinicians can acquire vital clues about the location and nature of the lesion. However, more advanced diagnostic techniques are necessary for accurate diagnosis and management.
Neuroimaging
Neuroimaging techniques, such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT), can provide valuable insights into the location and extent of the damage. MRI offers superior resolution of the brain and spinal cord, enabling the visualisation of demyelinating plaques in conditions like Multiple Sclerosis (UMN lesion) or the atrophy and degeneration in ALS (both UMN and LMN lesions).
Electromyogram and Nerve Conduction Studies
The Electromyogram (EMG) and Nerve Conduction Studies (NCS) are invaluable tools for diagnosing LMN lesions. While an EMG assesses muscle response to a nerve’s stimulation, the NCS measures the speed and strength of signals travelling between two points on a nerve. These studies can detect abnormalities in muscle and nerve function indicative of LMN lesions, such as those seen in ALS and peripheral neuropathy.
Lumbar Puncture
A Lumbar Puncture (or spinal tap) may be employed in certain cases to collect cerebrospinal fluid. Analysis of this fluid can reveal signs of inflammation, infection, or immune responses, particularly useful in diagnosing conditions like Multiple Sclerosis (UMN lesion).
Through these diagnostic techniques, clinicians can confidently differentiate between UMN and LMN lesions, guiding the prognosis and management of these conditions towards more personalised and effective treatments.
Functional Electrical Stimulation for ULM and LMN lesions
Electrical stimulation may be beneficial for lower or upper motor neuron lesions although the nature of delivery will be different.
FES Cycling such as that available via our RehaMove FES Cycling system allows a user to exercise weak or paralysed muscles for long term fitness. These systems connect a passive/active bike to a Functional Electrical Stimulation (FES) system in a way that synchronises the delivery of stimulation to the movement of the pedals. Versions of these bikes can support arm and shoulder exercise also.
This allows the user to recover and sustain muscle bulk and tissue quality despite their condition. A great deal of research supports the use of these systems with spinal cord injured persons as well as those recovering from a stroke or dealing with MS for example.
The objectives for use will vary depending on the condition. For example, persons with complete spinal cord injuries will use these bikes for long term cardiovascular function benefits as well as a reduction in overall complications from their condition. Users with MS may be able to prolong their walking abiliities.
The important point here is that to use systems such as the RehaMove system, the users LMN's must be intact.
Lower motor neuron injuries will generally prevent FES Cycling systems being used effectively.
Electrical stimulation can still be used with lower motor neuron injuries but the form of stimulation needs to be different. A lower motor neuron injury affecting a muscle will impact upon its nerve and tissue structure. As we described above, a LMN lesion can cause a flaccid type of paralysis that does not respond to the electrical stimulation forms delivered by most stimulators. The consequence of non-treatment is a gradual loss of tissue quality and a higher risk of secondary complications.
The local nerve supply to the muscle is lost so as long as muscle fibres are present, a form of stimulation can be used that works with the muscle fibres directly.
The RISE stimulator we work with at Anatomical Concepts is unique in that it can work with long standing and large muscles affected by a lower motor neuron lesion
The RISE stimulator can delivery the forms of electrical stimulation that use very long pulse widths and low frequencies combined with current levels up to 250 mA. Whilst some hand-held stimulation devices support "denervated" muscle, they are generally only suitable for small muscles typical of the uppoer limb.
For further details of how we use the RehaMove or RISE stimulator we have further reading on this site.
Conclusion
In conclusion, the differentiation between UMN and LMN lesions, although complex, is pivotal for precise diagnostic and therapeutic strategies. Advanced diagnostic techniques like neuroimaging, EMG, NCS, and lumbar puncture play key roles in this process. Furthermore, the employment of functional electrical stimulation systems such as the RehaMove and RISE stimulators offers promising results for muscle recovery and maintenance, provided they are used properly and thoughtfully based on the specific nature of the lesion. It is paramount for users to understand the type of lesion they have, as the effectiveness of these systems is dependent on the integrity of the lower motor neurons. As we continue to refine these technologies and our understanding of motor neuron lesions, we edge closer to more personalised, efficient, and empowering solutions for those affected by these conditions.
Related Articles
https://www.anatomicalconcepts.com/articles/how-to-use-the-rise-s
https://www.anatomicalconcepts.com/articles/evaluating-denervated-muscle-with-the-rise-stimulator
https://www.anatomicalconcepts.com/articles/claire-lomas-why-im-committed-to-fes-cycling
https://www.anatomicalconcepts.com/articles/what-is-fes-cycling