Transcutaneous Spinal Cord Stimulation (tSCS) - An Introduction for Non-Clinicians
Purpose and Intent
Transcutaneous spinal cord stimulation (tSCS) is a non-invasive technique that delivers electrical current to the spinal cord through electrodes placed on the skin overlying the spine. When used with people who have sustained a spinal cord injury (or perhaps another neurological condition), tSCS aims to activate neural circuits that may have become dormant or weakened following spinal cord injury.
The electrical stimulation increases the excitability of spinal nerve networks, making it easier for any remaining connections between the brain and body to transmit signals for voluntary movement. This priming effect is thought to create a more favourable environment for rehabilitation activities, potentially allowing individuals to achieve greater functional gains when tSCS is combined with intensive therapy.
Current applications include managing neuropathic pain, reducing spasticity (the muscle stiffness and spasms that commonly occur after spinal cord injury), and exploring the potential for enhanced motor recovery. Research continues to investigate the optimal ways to use this technology, with the goal of improving the quality of life and independence for people living with spinal cord injuries.
Ten Things You Should Know About tSCS
1. It is a non-invasive alternative to surgically implanted devices.
Unlike epidural spinal cord stimulators that require surgery to implant electrodes inside the body, tSCS works entirely through electrodes placed on the skin. This eliminates surgical risks such as infection, bleeding, and nerve damage, and makes the treatment more accessible to a broader range of people.
2. The stimulation primarily activates sensory nerve fibres in the spinal roots.
Research shows that tSCS works by stimulating the large-diameter sensory nerve fibres within the posterior (back) roots of the spinal cord. This increases the excitability of local spinal networks, which can help to unmask and enhance voluntary movements by capitalising on any functionally “silent” pathways that remain after injury.
3. tSCS can help manage chronic pain conditions.
One of the earliest applications of spinal cord stimulation was for pain relief. Studies have shown that tSCS can help reduce persistent pain that has not responded to conventional treatments, including phantom limb pain in people with amputations. Pain relief is typically achieved using a stimulation set below the level that causes muscle contractions.
4. It can reduce spasticity without medication side effects.
Spasticity, the muscle stiffness, spasms, and exaggerated reflexes common after spinal cord injury, can be significantly improved with tSCS. A single 30-minute session can produce immediate reductions in spasticity, with benefits lasting up to two hours. Regular application over six weeks has shown progressive improvements with carry-over effects lasting up to seven days. This offers a non-pharmacological alternative to medications that often come with unwanted side effects.
5. Best results often occur when tSCS is combined with rehabilitation therapy.
Research indicates that tSCS appears to work best as an adjunct to existing physical rehabilitation rather than as a standalone treatment. By priming the nervous system and increasing spinal excitability, tSCS may create a more receptive state for activity-based interventions. Studies have combined tSCS with walking training, robotic-assisted gait therapy, standing exercises, and upper limb rehabilitation with encouraging results.
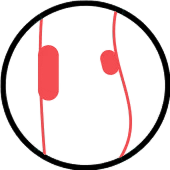
6. Electrode placement determines which functions are targeted.
The location of electrodes on the spine determines which neural pathways are primarily activated. Cervical placement (neck region) targets upper limb function, thoracic placement addresses trunk control, and lumbar placement (lower back, typically around T11-L2 vertebrae) targets lower limb function. The return electrodes are typically placed on the abdomen or over the hip bones.
7. There is ongoing debate about optimal stimulation parameters.
Different devices and research studies use varying stimulation settings. Most studies use frequencies between 30-50 Hz with pulse durations around 1 millisecond. Some systems use a high-frequency carrier wave (typically 10 kHz), which was initially thought to make stimulation more comfortable at higher intensities. However, recent research suggests that the carrier frequency may not provide significant comfort advantages over conventional stimulation and actually requires more energy to achieve the same neural activation.
8. The safety profile is generally favourable.
Studies report that tSCS is generally well tolerated. The most commonly reported issues are minor and temporary, including skin redness under electrodes and some discomfort at higher stimulation intensities. Some individuals experience tingling sensations (paraesthesia) during stimulation. Because it is non-invasive, tSCS can be discontinued immediately if any adverse effects occur, providing greater flexibility and safety compared to implanted systems.
9. Commercial devices are now available or in development.
While much early research used laboratory equipment, commercial tSCS devices are now emerging. The Arc-EX system from Onward Medical has been the subject of clinical trials and uses a high-frequency carrier approach.
This system is aimed at adults with a chronic, incomplete cervical spinal cord injury. The Up-LIFT trial in people with tetraplegia reported that about 90% of participants improved strength or function and around 87% reported better quality of life
The Stim2Go device from SensorStim Neurotechnology GmbH and Pajunk is now available in the UK with approved indications for neuropathic pain and spasm reduction. These developments are making tSCS more accessible for clinical use outside of research settings.
10. Research is ongoing and many questions remain.
Despite promising results, the evidence base for tSCS is still developing. Researchers continue to investigate the optimal stimulation parameters, which individuals respond best to treatment, and whether improvements are long-lasting or require ongoing use. Large-scale controlled trials are needed to establish definitive guidelines. It remains unclear whether the functional improvements seen in studies are due primarily to tSCS, the intensive therapy it is combined with, or a synergistic effect of both together.
Note: This document provides general information only and should not be considered medical advice. Individuals interested in tSCS should consult with qualified healthcare professionals