Stroke Awareness: Aiming for Prevention, Striving for Recovery
World Stroke Awareness Day is an opportunity to highlight this significant problem, learn about the signs and symptoms of a stroke, as well as bring a little hope to stroke survivors. As we discuss in this article, stroke is a serious and frequently seen event best prevented. We look at prevention, the signs and consequences of stroke and the topic of neuroplasticity, which has given rise to much optimism about the prospects for recovery. Finally, we look at some of Anatomical Concept's products relevant to stroke.
Stroke awareness is an important step toward prevention. We should focus on prevention but also tell the world that when the worst happens, our knowledge of effective treatment and rehabilitation techniques is improving all the time. Great progress is being made in making recovery possible for more stroke survivors.
Stroke can kill or lead to significant disability, thus we often hear the negative consequences of stroke. As rehabilitation specialists, we are involved in the provision of technology and services that can lead to recovery of physical, emotional and cognitive function. We know that intensive effort, know-how and technology can combine to achieve great things but resources have to be available and customised to the needs of the individual.
We often talk to stroke survivors who have been told not to expect too much recovery - some clinicians don't want to give "false hope". However, this can result in killing hope altogether. For many stroke survivors, hope feels like all they have at the beginning. We feel that hope can spur people into action and if correctly guided much can be achieved.
A wake-up call
A little while ago I needed some surgery. Not a massive deal; it was a day case with a local anaesthetic and I treated it as if I was going to the dentist. In other words, a chance to lie back and relax for a while.
Anyway, in surgery preparation I had my blood pressure taken and was shocked to find that it was 160 over 80. Ok, the protocol followed to take my blood pressure wasn't the best - and I could rationalise that this one reading was probably not remarkable for someone in their 70s, but I have always strived to keep fit. This was not expected and somewhat disconcerting.
One challenge of being involved in healthcare is we have a clearer picture than most of what is likely to kill us. We can look at our genetic inheritance, factor in our lifestyle and consult those actuarial tables. High blood pressure is a serious risk and should not be ignored as it is a risk factor for stroke and a number of other conditions.
One of my favourite medical authors is Dr Peter Attia who focuses on longevity - his podcast "The Drive" is exceptional for its quality and depth of content.
Peter tells the story of being at medical school and being asked the question,
"What is the most common presentation (symptom) of heart disease?"
Most people would think it is chest pain, left arm pain, shortness of breath and so on.
In fact, it is sudden death.
Basically, we get to know the patient has heart disease because he just died from it. It's not unreasonable to suggest the person who knows cardiovascular disease best is the pathologist.
Striking a lighter tone, we can say that mortality rates from the first surprise heart attacks have dropped in recent years although they are still fatal around one-third of the time. Heart disease and stroke, which we should think of together as atherosclerotic cardiovascular disease (ASCVD) still represent a major cause of death. In the USA for example, approximately 2,300 persons per day will die from this cause. The figure is around 110 in the UK. Equally shocking is the fact that American women are up to ten times more likely to die from ASCVD than breast cancer. It makes sense to focus on prevention whenever possible and being alert to the signs of a stroke.
Recognising the Signs of a Stroke
A key aspect of stroke awareness is the widespread recognition of the symptoms of a stroke. In the UK we have had a widely publicised campaign referred to as the FAST (Face, Arm, Speech,Time) campaign. This highlights the following three elements of the signs of stroke:
Facial weakness - can the person smile? Has their face drooped?
Arm weakness - can the person raise both arms?
Speech problems - can the person speak clearly and understand what you say?
If any or all of these elements are present, then urgent, timely action is required.
In addition to these three, there are actually a number of other signs of stroke onset. These can include sudden weakness or numbness on one side of the body, loss of balance and coordination, confusion and trouble speaking or understanding speech. It is important to educate ourselves and those around us about these signs so that we can take prompt action in case of a stroke. Timely intervention can significantly reduce the risk of disability and death.
In recent weeks a petitioner has called on the Scottish Parliament to urge the Scottish Government to increase public awareness of the systems of stroke and review the FAST stroke campaign to ensure that it includes all the symptoms of a potential stroke.
Anthony (Tony) Bundy tragically lost his life on 29th June 2023 after suffering a Basilar Artery Ischaemic Stroke. When Tony started suffering a stroke, his face and arms were unaffected and his speech was not slurred. This meant that Tony passed the "FAST" stroke test, and was denied the emergency treatment required to save his life until it was too late.
Tony's family are now raising awareness of all the symptoms of stroke, including the inability to stand, cold sweats, eyes struggling to focus, slowed speech, nausea and vomiting.
They are calling for a review of the FAST stroke campaign, looking at international examples, in order to ensure stroke awareness campaigns include a wider range of symptoms of stroke. This is intended to maximise knowledge amongst the general public and the medical profession.
Increasing awareness will hopefully mean fewer families will have to experience the pain and loss that Tony’s family has endured. The Scottish Government's Stroke Improvement Plan now has a priority to establish the current degree of public understanding of the symptoms of stroke, and whether certain at-risk groups need a different form and scope of messaging.
Focusing on Prevention
An important question is "Can strokes be prevented?". The best way we know to prevent a stroke is to make healthy lifestyle choices. This includes:
Healthy food and diet
Eating a healthy diet. This is actually a complicated topic in its own right but the "standard" advice will suggest eating plenty of fruits, vegetables and whole grains, and limiting processed foods, saturated and trans fats. You and I will see lots of dietary advice and "fad" diets but we should be cautious. Obesity is widespread and largely influenced by diet so either people ignore advice or it isn't effective.
Exercising regularly. There is no doubt about the benefits of exercise although we could debate what type and how much to aim for. The "standard advice" is to aim for at least 30 minutes of moderate-intensity aerobic activity most days of the week. I personally think that strength training is also essential for all round physical and metabolic health. It's important to note that exercise is not
Maintaining a healthy weight. What represents a healthy weight we could also debate as body composition is what matters. Our body weight is influenced greatly by our diet and to a lesser extent by exercise.
Quitting smoking. No doubt about this one. It's bad for your overall health and will increase the risk of stroke. Smoking is a major controllable risk factor for ASCVD.
Limiting alcohol intake. Again, you probably know this one already but excessive drinking can raise blood pressure, which increases the risk of stroke. Despite some popular literature there really isn't a safe level of alcohol consumption.
Leading an active lifestyle can help reduce the risk of stroke.
In addition to these lifestyle changes, it is important to manage any underlying medical conditions that will increase your risk of stroke, such as high blood pressure, high cholesterol and metabolic disorders such as diabetes. If you have a family history of stroke or other risk factors, it is important to talk to your doctor about your personal risk of stroke and what you can do to reduce it. When you have known risk factors it's important to get regular checkups and take any medications that have been prescribed.
It's also important to manage stress. Stress is unavoidable to some extent but can be unhealthy and can increase your blood pressure and risk of stroke. Our autonomic nervous system is an important part of our physiology for maintaining "balance" and dealing with stress but in evolutionary terms is best suited for short episodes of stress. Many of us will have heard of our "fight or flight" response which is part of our autonomic nervous system's process for dealing with sudden stress. It was great for dealing with the sight of a Sabre Tooth Tiger when we lived in caves. It does not work so well when stress is more subtle and unremitting. We tend to get "stuck" in a stressed and unbalanced situation that results in many undesirable consequences for health and wellbeing.
I know it's not always easy, but we should always seek healthy ways to manage stress, such as exercise, applying relaxation techniques and spending time with loved ones. Going for a daily walk is a great way of exercising, relieving stress and even getting some perspective on life's problems.
By making healthy lifestyle choices and managing any underlying medical conditions, you can significantly reduce your risk of stroke.
A New Perspective on Stroke
It's important to understand that stroke is not just a condition that affects the elderly. It can happen to anyone, at any age. And while prevention is key, it's also important to keep in mind that stroke recovery is more achievable than ever before given the right types of intervention and a commitment to rehabilitation.
In addition to traditional physical therapy and rehabilitation methods, technology is now playing a major role in helping stroke survivors regain function. From virtual reality to robotic devices, these advancements have shown great promise in improving motor skills, speech and cognitive function. Recognising this potential for recovery is important as it gives hope to those who may feel discouraged or hopeless after a stroke.
As rehabilitation specialists, our goal is to provide personalised technology and treatment plans that combine intensive effort, technology and know-how to achieve the best possible outcome for each individual.
Consequences of a Stroke
As we discussed above, the most serious consequence of a stroke or ASCVD is sudden death. It's important for us all to know the signs and symptoms of stroke and do all we can to ensure prompt medical treatment.
As we approach World Stroke Awareness Day, we can reflect on the physical, cognitive and emotional consequences of being a stroke survivor. As we will see the consequences can be profound but many people can make significant recoveries with the help of rehabilitation and support.
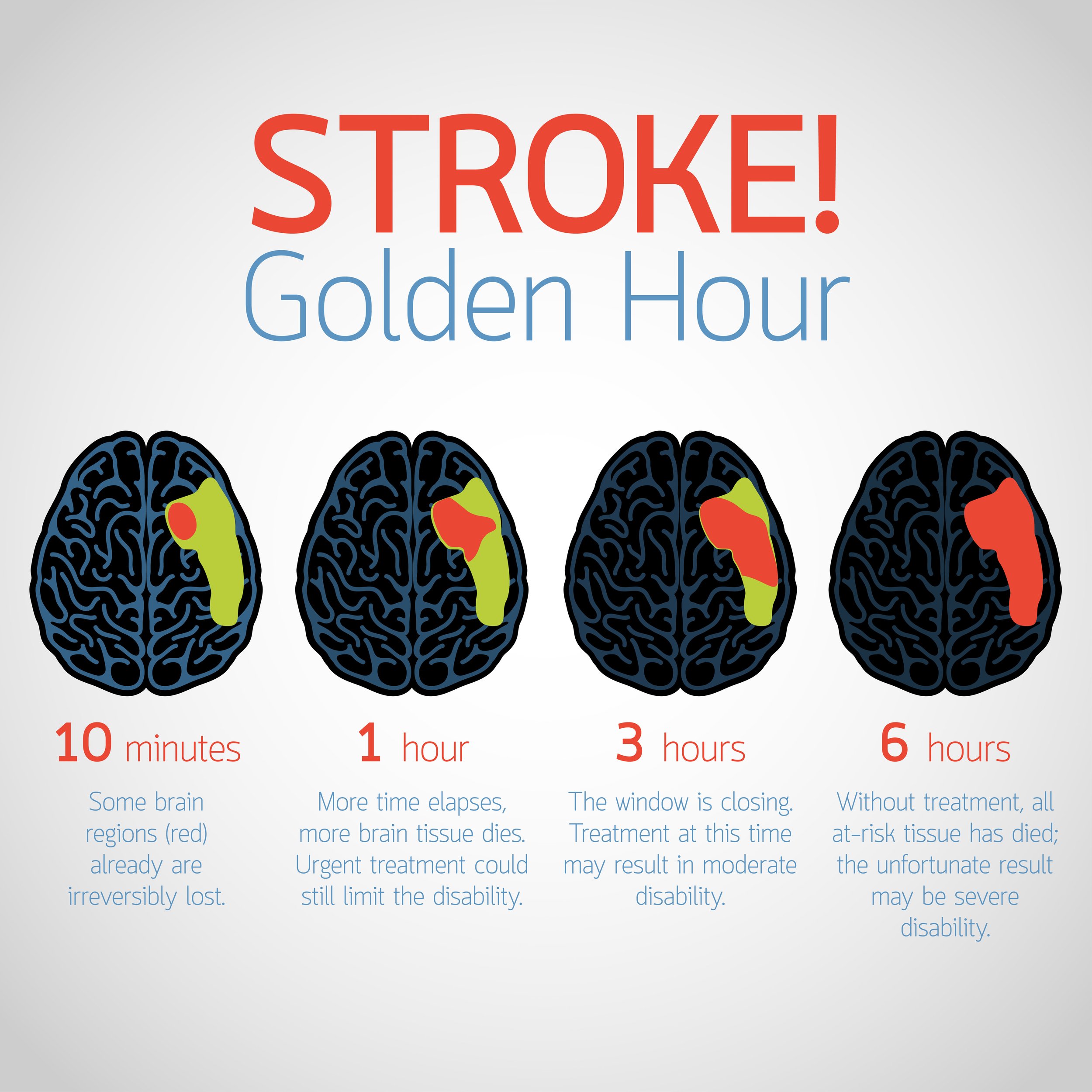
A stroke occurs when the blood supply to part of the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. Within minutes brain cells begin to die with severe consequences. Depending on the location and severity of the stroke different functions such as movement, speech and memory can be affected. The degree of disability also varies greatly from person to person.
As we will see, in addition to physical challenges, many stroke survivors may also experience emotional and psychological difficulties such as depression, anxiety or changes in personality. These issues can make it difficult for survivors to adjust to life after a stroke.
Physical consequences of stroke
Some common physical consequences include:
Weakness or paralysis on one side of the body
Loss of coordination
Difficulty with balance and walking
Difficulty speaking or swallowing
Vision problems
Fatigue
Incontinence
At Anatomical Concepts, we are mostly focused on physical rehabilitation. The temptation is for people after a stroke to focus on an issue in isolation. In other words, look to fix something that bothers them the most. Usually, it is wise to step back and think about broader goals first. What will have the greatest impact on lifestyle and independence? What disabilities might we try to recover from and which might we need to compensate for?
Cognitive consequences of stroke
Cognitive consequences of stroke can be just as significant as physical ones and include difficulties with thinking and memory, attention and concentration, problem-solving and judgment and much more.
Emotional consequences of stroke
Emotional consequences of stroke can include depression, anxiety, irritability, sadness, anger and social isolation.
Prospects for Recovery
The body is a fantastic machine that can self-regulate its thousands of processes without a conscious thought from us. It can adapt to changes in the demands we place upon it as well as a range of changes in its environment. A stroke disrupts this to varying degrees but even then it will try to work around issues and get back to business as usual. In some cases restitution takes place and recovery is largely complete - but certainly, in most cases, recovery will not be complete and assistive technology may be useful.
As a student looking at stroke recovery prospects in the 1970s, we expected recovery prospects to plateau after around six months post-stroke. Most stroke survivors were expected to make some spontaneous improvement in their physical function but many were expected to have some residual weakness or paralysis after that initial six months. We knew anecdotally that intensive, exercise-based therapy might help in some cases but this was before anyone was talking about neuroplasticity.
Stroke recovery expectations in the 1970s in the USA and UK were much less optimistic than they are today. This was due to a number of factors, including:
Less advanced medical imaging techniques made it more difficult to rapidly diagnose strokes and assess the severity of the damage.
There were fewer effective treatments for stroke.
Rehabilitation techniques were less sophisticated.
Restitution and Compensation
The theory and practice of rehabilitation has been to use therapy to recover as much as possible (restitution) and then use assistive technology if necessary to compensate for what could not be recovered.
These days we see improved prospects for recovery. As stroke is so individual it is difficult to generalise on recovery prospects but we have seen persons many years post-stroke achieve useful functional recovery that would have once been thought of as impossible.
Cognitive recovery was generally considered to be more limited than physical recovery. Stroke survivors with cognitive impairments were often expected to need long-term support with activities such as managing their finances, planning their daily activities and remembering to take medications. The aim would be to compensate for loss of function by using assistive technology such as memory aids.
At Anatomical Concepts, we much later came to understand that cognitive functions too could recover and be enhanced with intensive computer-based training. The RehaCom software developed in Germany by Hasomed GmbH becoming our offering in this area. Computer based training has been slow to be accepted in the UK despite a good evidence base from Germany, Asia and the USA.
Emotional recovery was also recognised as an important part of stroke rehabilitation. However, there was less understanding of the emotional challenges faced by stroke survivors and their families in the 1970s. Today there is much greater recognition of this - and indeed perhaps the sources of hope are greater.
I believe that physical, cognitive and emotional issues are not siloed - each one will tend to affect the others for better or worse.
Despite the less optimistic expectations for stroke recovery in the 1970s, many stroke survivors made significant improvements with the help of rehabilitation and support. Today, stroke recovery expectations are much more optimistic, thanks to advances in medical imaging, treatment and rehabilitation techniques.
It is important to note that stroke recovery remains a highly individualised process and some people make full recoveries, while others have lifelong disabilities. The severity of the stroke, the age of the person and their overall health all play a role in recovery.
Neuroplasticity - A Cause for Hope
I mentioned above that our bodies are wonderful self-regulating machines that can rise above many of the issues that disrupt our health. Neuroplasticity is a term that is often used (and sometimes misused) today. It points to the fact that neurological body systems can be provoked to adapt, recover and learn new functions many years after an injury and even when we are elderly.
As we have seen, neurological conditions such as a stroke can result in a vast array of functional deficits. The emergence of neuroplasticity as a rehabilitation topic has given rise to much optimism about the prospects for functional recovery in rehabilitation; far beyond what we previously might have expected would be possible even a few decades ago.
Neuroplasticity is defined as the potential for functional and anatomical changes of the nervous system in response to stimuli during learning or in response to injury (Kandel et al, 2013).
In other words, it’s about the central nervous system’s apparent ability to rewire its neural circuitry to make adaptive changes. It suggests that in some circumstances this can allow for functions affected by a stroke to be relearned and recovered.
In the popular literature, neuroplasticity is generally looked upon as a positive thing but this is not always the case. It's a learning process and as such is subject to both positive and negative influences.
When we walk, two sources of information must flow and are processed. One comes from "above": instructions from the brain about where we want to go based on what we see. The other comes from below: sensory information from the muscles, tendons and skin. After a stroke, the communication lines between the brain and body are cut or dramatically diminished, depending on the severity of the event.
Doctors and researchers once thought it impossible for us to regain any type of control over the limbs without coherent instruction from the brain but unlike fixed mechanical circuits, the brain and spinal cord, as it turns out are malleable. Connections between neurons can grow or atrophy based on activity. Neuroscientists have now overthrown the age-old dogma that the adult brain can’t change.
The relatively recent exciting discovery that the nervous system is plastic and adaptable even in adulthood is a source of great hope to people with disorders of the central nervous system such as stroke. Neuroplasticity has led to promising new treatments for a range of conditions and as we learn more, neuroplasticity should continue to lead to progress in rehabilitation.
The power of practice helps to regain function after a stroke.
The basic idea is that if we can practise a movement in a particular way, we might recover lost function at least in part. For example, a person whose arm movement is affected by stroke might be able to recover useful function provided they can practise the required movement often enough. The flip side of this is we must ‘use it or lose it’.
Currently, repeated practice and specific training provide the best opportunities to reverse the maladaptive plasticity associated with neuropathology and promote instead the adaptive plasticity supportive of function. We can become a victim of the nervous system’s plasticity if we don’t act to take advantage of it but much is still unknown about how to optimise this.
Evidence suggests that several non-invasive clinically accessible forms of energy can be a source of useful stimulus (Robertson et al, 2006). Electrical, magnetic and vibration stimuli may be used to augment the effects of training.
In essence, stimulation activates the same neural circuits that are activated by training, and when used in combination with training, stimulation has the potential to promote neuroplasticity beyond that achieved by practice or training alone. Studies involving neurologically healthy individuals have shown these approaches to enhance neural excitability and motor performance. Non-invasive, clinically available, forms of stimulation may be used to modulate neural excitability as an adjuvant to programmes designed to improve hand/arm or walking function in people with neurological disorders.
How to Provoke Useful Neuroplasticity
There are several factors commonly involved in motor learning and hence neuroplasticity. To some extent, they overlap:
Carrying out a skill practice that is challenging, but not too difficult.
Practice should be specific.
Skill practice must be intense.
Practice should be progressive.
Timing matters.
Engage motivation to enhance the learning.
Let’s describe each of these in more detail. Research evidence shows that the difficulty of the task matters to the process of learning (Magness, 2022). The challenge is how to create a situation where practice is difficult and cognitively engaging but not impossible.
Specificity effects have been recognised in learning research for more than 100 years, the general finding being that the transfer of skills from practice to real-world application will be small unless the skills required are nearly identical. What this means is that general exercise and activities like strength training for recovery are most effective when combined with task-specific training programmes. Research is now looking at how practice in one task can transfer to another task in a meaningful way.
What do we mean by ‘intense’? Intensity implies that some combination of the dose, frequency and duration of training practice is important to get results. Although this suggestion is supported by research results, there is a lack of detail when we try to pin down what exactly is a necessary and sufficient level of intensity for an individual case.
Some researchers point out that being able to tap into someone’s motivation to practise may be more effective than simply cranking up the intensity of the practice. The idea here is that focusing on practice simply to reduce impairment is less motivating than looking at seeking benefits that directly impact the person’s quality of life.
There is no doubt that repeated attempts to solve a motor-control task benefit neuroplasticity and motor learning, but tasks must not be too simple or repetitive. Simple tasks well within the capability of the performer will not induce neural plasticity. What’s needed could be described as ‘repetition without repetition’.
Imagine learning a golf swing that involves lots of repetition. Let’s say you have been taught well and don’t see learning the golf swing as just rapidly hitting 1,000 golf balls down the driving range. For each stroke, you learn to follow the same thoughtful process with careful setup and attention to detail. However carefully you try to replicate each golf swing, there are going to be lots of small deviations in muscle and limb joint activity, and so on. What seems like exact repetition is not exactly so but over time, you may consciously learn from your results and refine your swing.
When it comes to robotic systems that allow repetitive practice, perhaps the same observations hold. For example, the iCONE robot for upper-limb rehabilitation allows the user to practise arm movement guided within an adjustable ‘haptic tunnel’. This allows the task to take place repetitively without constraining the movement to be the same with each repetition. Over time, the haptic tunnel’s size can be adjusted as the user’s performance improves.
Different forms of plasticity occur at different times during training. This implies that the timing of an intense therapy programme is important. Some researchers are advocating early interventions, for example in the first month after a stroke. This seems to make sense, but a lot of stroke research has only been carried out in the chronic phase of recovery. This is because research in the earliest stages is fraught with difficulty and ethical concerns.
Many therapeutic interventions rely on extrinsic motivation to be effective. It seems to me that the best results come when motivation is intrinsic and the person’s mindset is adjusted to provide a consistent drive to work at improvement.
We have seen that neuroplasticity is a natural process that we hope to take advantage of or suffer the consequences. It can be the source of potential improvement in function, but if we do nothing, we will see the body’s ‘use it or lose it’ process at work.
Neuroplasticity has not only revolutionised our approach to stroke rehabilitation but also instilled a sense of optimism and hope. It has reaffirmed the possibility of recovery and improvement, irrespective of the severity of the stroke and the stage of recovery.
I wrote a couple of articles on the topic of neuroplasticity
"What is neuroplasticity and why should I care?"
This article discusses in more detail what neuroplasticity is and how it can be used to treat brain injuries. The article also reveals the different factors that can affect neuroplasticity, such as the intensity and duration of practice. The article emphasizes that the timing and intensity of practice are important factors to consider when trying to promote neuroplasticity.
and "Bridging the Gap: Why neuroplasticity matters"
This is an article about neuroplasticity and how it can be used to improve rehabilitation. It discusses how it can be harnessed to promote recovery after injury. The article also details some of the factors that can influence neuroplasticity. Some of the important points from this article are that neuroplasticity is greatest early in the recovery process and that intrinsic motivation is often a key to success.
Anatomical Concept's Products for Stroke
We have seen that recovery from a stroke is often possible to some extent but can take intensive effort of the "right" kind following a realistic assessment of the potential for recovery. We gave a sort of recipe for neuroplasticity above, but we are still trying to establish the necessary and sufficient ingredients to give the best approach for each individual.
The products we deal with which we believe are relevant to stroke, include the following which can contribute to the restoration of particular functions.
RehaMove FES Cycling system
RehaMove FES Cycling. An FES bike involves using functional electrical stimulation (FES) synchronised with the movement of the pedals of a passive/active bike. This can help with the "one-sided" weakness often seen following a stroke. A stroke survivor may be able to pedal this type of bike to exercise for a brief period but is likely to quickly fatigue. This technology senses the user’s contribution and stimulates the leg and or arm muscles to encourage them to recover strength over a period of time. Sometimes the stimulation is applied just to the affected side and sometimes to both limbs.
Sequence Mode FES application. The FES unit we use with the RehaMove FES bike comes with a powerful application called "Sequence Mode". This allows the user to create a powerful stimulation programme that can be customised to the needs of the user for training or assistive purposes. Examples might be to activate muscles at the right time during walking training or to relax tight muscles that are limiting movement.
NexStride with the laser cue
NexStride. The product provides a visual and auditory cue to encourage a regular walking pattern. Whilst commonly used by persons with Parkinson's who can suffer from the freezing of gait, NexStride has proved to be a valuable training aid for persons recovering from stroke. This is because the cueing line and rhythm allow the user to work around the damage in their nervous system.
Carbonhand glove
Carbonhand. This is a robotic glove technology that can assist users with a weak grip. One-sided weakness is a common consequence of a stroke. The development of the Carbonhand by Bioservo Technologies has been refined from work carried out originally to support manual workers who are prone to repetitive strain injuries.
This truly novel product uses a glove with sensors placed on the fingers and parts of the hand. The control unit can sense the user’s intention to grip an object by its contract with these sensors and this information is used to instantly activate the grasp. The strength, speed and sensitivity of the grip can all be adjusted for different practical situations via an App. Like most assistive technology, this product will not be suitable for everyone but can be life-changing for those who can use it.
Sadly, these items may not generally be available from the NHS and this is a barrier for many persons following a stroke.
The PRAFO (Pressure Relief Ankle Foot Orthosis) can have an important role in the early phase of stroke.
In addition to preventing heel pressure ulcers, these orthoses can be important in allowing early mobilisation of patients following a stroke. Contractures can rapidly occur in persons who are immobile in bed due to muscle imbalances. Muscle imbalances after a stroke can lead to an equinovarus contracture in which it becomes difficult to place the foot in a neutral position.
This is a problem for continuity of care because such a contracture can prevent the patient from being mobilised and this leads to greater disability and delayed rehabilitation. The PRAFO's metal heel connector and structure can help prevent such equinovarus contractures and keep the patient protected from early walking. The structure can also be connected to a knee orthosis when necessary for the rehabilitation of walking.
Conclusion
In support of Stroke Awareness Day, we have looked at stroke, its signs and symptoms, plus prevention and its consequences. We also recognised that advances in rehabilitation now are leading to greater prospects for recovery.
Neuroplasticity has the potential to greatly impact stroke rehabilitation and recovery. With our understanding of this natural process, we can develop effective therapeutic interventions and technologies to harness its power for improved outcomes. At Anatomical Concepts, we offer a range of products designed to aid in stroke recovery by targeting specific impairments and promoting neuroplasticity.
Our goal is to provide individuals with the tools they need to reach their full potential and regain function after a stroke. Let’s continue to explore and utilise the power of neuroplasticity for the benefit of those who have experienced a stroke, empowering them on their journey towards recovery. So don't lose hope but rather embrace the possibilities that neuroplasticity offers for stroke rehabilitation.
Additional Reading
Dr Peter Attia podcast, "Drive" see https://peterattiamd.com/
Kandel, E; Koster, J; Mack, S; Siegelbaum, S (2013)
Principles of Neural Science (fifth edition). McGraw-Hill
Magness, S (2022) Do hard things: Why we get resilience wrong and the surprising science of real toughness. Harper Collins
Robertson, V; Ward, A; Low, J; Reed, A (2006) Electrotherapy Explained: Principles and practice. Elsevier Health Sciences
"Making a habit of training for physical recovery"
This is an article about making a habit of training for physical recovery. It discusses the importance of neuroplasticity and how athletes train to succeed. The article also details the steps required to build adherence to a training program. Some of the important points from this article are that motivation is key to starting a training program, but discipline and habit are necessary to achieve long-term goals.