Why Pillows Fail: The Biomechanics of Heel Suspension
The pillow remains perhaps the most commonly used heel elevation method in hospitals worldwide. I guess this is because they are readily available, cost nothing beyond what's already supplied for patient comfort, and require no special equipment or training. They are also inadequate for heel protection and can compromise continuity of care.
The evidence is now clear: an Australian multi-centre ICU trial found that purpose-designed heel offloading devices achieved a 0.4% pressure injury incidence, compared to 8.4% with standard care, which typically means pillows and repositioning [1]. That's a twenty-fold difference. Translated into practical terms: for every 1,000 patients, 79 fewer will develop heel pressure injuries when proper offloading devices are used instead of pillows.
This isn't a criticism of clinical staff who use pillows—they're working with what's available and following long-established practice. It's an observation about biomechanics: what a pillow can and cannot achieve when the goal is heel offloading.
Understanding why pillows often fail points toward what effective heel protection actually requires.
The goal is heel floating, not elevation.
Pillows are best used for their original application.
The 2025 International Pressure Injury Guideline specifies that heels should be "fully free from contact with the support surface" [2]. The recommendation is explicit: use a heel-offloading device that provides complete suspension.
This is a precise biomechanical state: the heel suspended in space, contacting nothing, with no pressure or shear acting on the tissue.
The heel is particularly vulnerable to pressure injury. Research shows that heel tissue deforms by 30-40% under body weight—substantially more than the sacral region, which deforms 20-25% [3,4]. The anatomy creates concentrated mechanical stress: a prominent calcaneus covered by minimal subcutaneous fat, with no muscular cushioning to distribute load. This is why the heel is a high-risk site, second only to the sacrum for pressure injury incidence.
Elevation is not the same as floating. A heel can be elevated—raised above the mattress level—while still in contact with a surface. If that surface exerts pressure on the heel tissue, the elevation has moved the heel without achieving offloading.
The distinction matters because the goal isn't geometric (raising the heel) but mechanical (eliminating tissue load).
Pillows compress under load.
Standard hospital pillows are designed for comfort, not pressure elimination. They're filled with soft materials—polyester fibre, foam, or down alternatives—that compress when weight is applied.
When a leg rests on a pillow:
1. The pillow initially elevates the leg
2. The weight of the leg compresses the pillow filling
3. The pillow progressively flattens
4. The heel sinks toward the mattress
5. Eventually, the heel contacts either the compressed pillow or the mattress beneath it
Compression occurs gradually, often while the patient is sleeping or sedated. A pillow that appeared to suspend the heel at 10 pm may have flattened sufficiently by 2 am that the heel is bearing pressure again.
The critical issue is the timeline. Kosiak's foundational research established that microscopic pathologic changes occur in tissues subjected to pressure for as little as one hour, providing the basis for two-hour repositioning protocols [5]. High tissue deformations cause microscopic cell damage within minutes, though the visible damage may take hours to become clinically apparent. A pillow that loses its loft during a single night shift exposes the patient during exactly this vulnerability window.
The degree of compression depends on pillow quality, fill type, and the patient's leg weight. But all pillows compress to some extent. It's inherent to their design.
Pillows shift position.
Even if a pillow maintained its loft perfectly, it would still face a second problem: positional instability.
Pillows are not fixed in place. They move when:
- The patient moves, even slightly
- The bed is adjusted (head elevation, knee break)
- Staff perform care activities (repositioning, washing, dressing changes)
- The patient is turned for pressure relief elsewhere
A pillow that was correctly positioned to float the heel may shift during any of these activities. Unless someone checks and corrects the position, the heel may end up resting on the pillow in a pressure-bearing configuration, or on the mattress entirely.
The international guidelines explicitly acknowledge this problem. They recommend that clinicians "regularly check and readjust pillows to ensure the heel remains offloaded" and "use a hand check underneath a heel offloading device to check the heel is 'floating' above the full body support surface" [2]. They also warn that adding pillows under the knee when using a heel device can cause the heel to contact the bed surface, rendering the device ineffective.
In busy clinical environments, continuous pillow monitoring isn't feasible. The pillow positioned by the evening shift may not be checked until morning handover, eight or more hours during which shift, and compression may have compromised the offloading effect. A 2024 ethnographic study on English orthopaedic wards observed that heel devices "were not viewed as suitable for every patient at every point in their hospital stay," with clinical staff emphasising the challenge of identifying suitable at-risk patient groups capable of maintaining device use [6]. The same problem applies even more acutely to pillows, which require more frequent intervention.
Partial contact isn't offloading.
Sometimes a pillow elevates most of the heel but allows partial contact—perhaps the posterior edge of the calcaneus resting on the pillow surface while the rest floats.
This partial offloading is better than full contact but falls short of the guideline recommendation. Pressure injury risk relates to the tissue that is loaded, not the tissue that isn't.
If one square centimetre of heel is bearing pressure while the rest floats, that one square centimetre is at risk. The injury will develop where the load concentrates, regardless of what's happening elsewhere.
Complete offloading means complete—no contact at all. Partial solutions leave partial risk.
Shear forces persist with pillow use.
Pressure acts perpendicular to the tissue surface. Shear acts parallel to it—the sliding or stretching of tissue layers against each other.
Shear is particularly damaging because it stretches the blood vessels that run between tissue layers, occluding blood flow even at relatively low perpendicular pressure. The research here is compelling: Bennett and colleagues demonstrated that shear can reduce the pressure threshold for blood occlusion by nearly 50% [7]. In other words, the combination of pressure and shear is not additive but multiplicative—tissue damage occurs at much lower pressure levels when shear is present.
Mak and colleagues found that frictional shear increased susceptibility to skin breakdown at pressures as low as 67 kPa, and that greater pressures alone did not cause additional ulceration without shear [4]. As their research summary puts it: "Shearing stops or reduces blood flow more easily than pressure alone."
When a heel rests on a pillow surface:
- Skin adheres to the pillow cover through friction
- Deeper tissues may shift relative to the skin when the patient moves
- This creates shear stress on the blood vessels between layers
- Even without high perpendicular pressure, perfusion can be compromised
True heel floating eliminates shear because there's no contact surface for the skin to adhere to. No contact means no friction means no shear.
Pillows, even when raised, don't eliminate the shear problem. Every time the patient moves, or the bed position changes, or the pillow shifts, the heel skin experiences shear against the pillow surface. This explains why partial offloading—reducing pressure without eliminating contact—remains a risk.
The evidence confirms pillow limitations.
Research comparing different heel protection approaches provides empirical confirmation of these biomechanical observations.
A systematic review by Greenwood and colleagues evaluated 15 randomised controlled trials and found that heel offloading devices reduced Category 2 and above pressure injuries by over 90% (relative risk 0.08; 95% CI: 0.01-0.67) [8]. The Australian multi-centre ICU trial by Barakat-Johnson and colleagues reported a hazard ratio of 0.0896 for patients using heel-offloading boots compared with standard care—a statistically significant reduction (p = 0.0239) [1]. Notably, injuries in the device group were Stage 1 (superficial), whereas those in the control group were Stage 2-4 (more severe).
The comparative trial data is stark: heel offloading boots achieved 0.4% injury incidence versus 8.4% with standard care (which typically includes pillows as the primary intervention) [1]. The twenty-fold difference reflects the gap between true offloading and conventional approaches.
One caution: not all devices are equal. Some poorly designed "offloading" devices have performed worse than pillows in comparative studies, which is why the international guidelines recommend specifically designed devices appropriate to the individual's mobility and activity level [2]. Design quality matters.
Pillows aren't useless—they're better than nothing. But "better than nothing" isn't the standard we should accept when more effective options exist. For Stage 3 or greater heel pressure injuries, the guidelines are explicit: specifically designed heel suspension devices are recommended—not pillows or foam cushions [2].
The economic reality.
For case managers, legal professionals, and healthcare commissioners, the cost-effectiveness argument is straightforward.
UK NHS data indicate the treatment cost of pressure injuries by severity [9,10]:
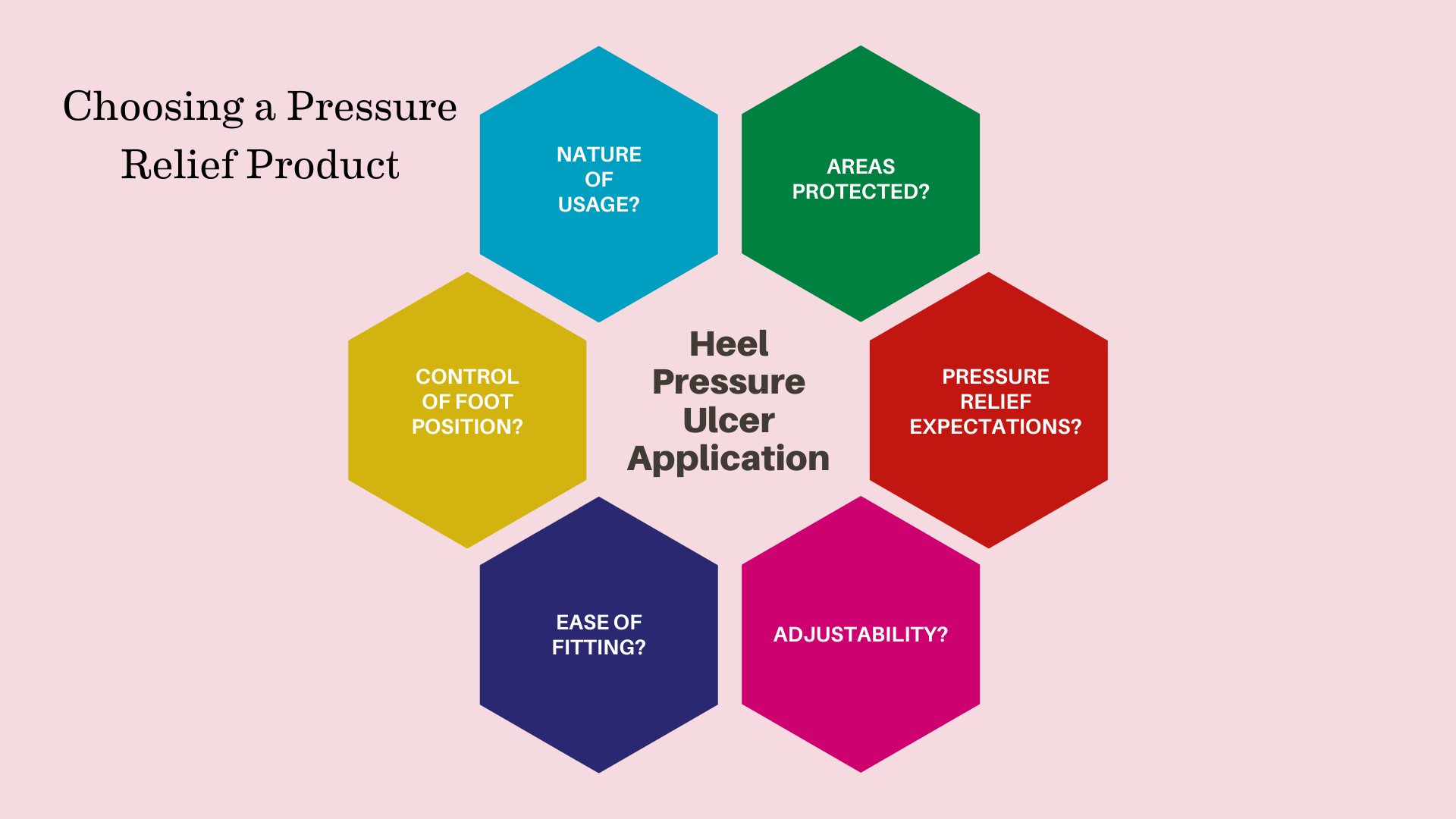
There are a number of factors to consider when choosing a pressure relief product.
- Grade 1: approximately £1,000-£1,214
- Grade 2: £3,649-£5,241
- Grade 3: £7,313-£8,722
- Grade 4: £10,551-£14,108
Hospital-acquired pressure ulcers extend stays by 4-8 additional days on average. The NHS burden is estimated at £1.4-2.2 billion annually—representing up to 4% of total NHS expenditure [9]. Litigation damages have reached £21-23.5 million in recent years for pressure ulcer cases alone.
NICE cost-effectiveness analyses demonstrate that heel protection devices dominate standard care economically—meaning they provide better outcomes at lower total cost when treatment expenses are factored in [11].
The arithmetic is compelling: a single prevented Grade 4 heel ulcer pays for dozens of prevention devices. The Prafo range can act to prevent ulceration, and the costs are modest. This isn't an argument for spending more—it's an argument for spending differently.
What effective offloading requires.
Given the limitations of pillows, what would an effective heel offloading device need to provide?
Structural integrity under load. The device must maintain its shape and position when supporting the weight of the leg. No compression, no flattening, no gradual failure over time.
Positional stability. The device must remain in place despite patient movement, bed adjustment, and care activities. It shouldn't require continuous monitoring and repositioning.
Complete heel suspension. The device must hold the heel entirely clear of all surfaces—the mattress, the device itself, and any other contact points. Partial offloading isn't sufficient.
Shear elimination. By achieving complete suspension, the device eliminates the contact that generates shear forces.
Extended durability. The device must function effectively over days, weeks, or longer—the full duration of the patient's vulnerability period.
Patient tolerance. Evidence shows that well-designed devices are worn significantly longer. Preliminary adherence data suggest patients wear well-designed devices 63% longer per day (13.7 hours versus 8.4 hours), with "never wear" rates of 12% versus 40% [12]. A device that patients won't wear provides no protection.
The Prafo range achieves these requirements through engineering rather than soft materials. The metal upright structure doesn't compress. The design cradles the calf and foot while suspending the heel in a fixed position. The construction maintains this configuration reliably over extended use.
A note on pillow technique.
Some clinicians have developed pillow techniques that improve on basic application—lengthwise positioning along the calf, specific arrangements to create a "bridge" under which the heel floats, and regular repositioning protocols.
These techniques can improve outcomes compared to casual pillow use. They represent clinical skill applied to imperfect tools.
However, they remain dependent on:
- Correct initial positioning
- Pillow quality is sufficient to maintain the position
- Regular checking and repositioning
- Staff knowledge of the technique across all shifts
In busy clinical environments, technique-dependent solutions are vulnerable to variation, skill gaps, and time pressures. A solution that achieves offloading through device design rather than technique reduces this variability.
The standard is floating heels.
The 2025 International Pressure Injury Guideline establishes the standard: heels "fully free from contact with the support surface" [2].
This is what prevention looks like. This is what the evidence supports. The evidence strength is rated as conditional with low certainty—not because the effect is uncertain, but because the research is still developing. The effect sizes are substantial: a 90%+ reduction in Category 2+ injuries [8], a twenty-fold difference in incidence rates [1].
Pillows, despite their widespread availability, often fail to meet this standard. They compress. They shift. They allow partial contact. They don't eliminate shear.
This isn't an argument for abandoning pillows in all circumstances—resource constraints are real, and imperfect prevention is better than none. When pillows must be used, the guidelines are specific: one pillow under the whole length of each calf (one pillow per leg), positioned below the popliteal fossa, with regular checking and readjustment. Do not use sheets or pillowcases on devices, as this creates a "hammocking effect" [2].
But these are workarounds for an imperfect tool. For patients at genuine risk—ICU patients who are almost four times more likely to develop pressure injuries [1], post-surgical patients, those with reduced sensation or mobility—purpose-designed offloading devices represent evidence-based practice.
Prevention that reliably achieves the guideline standard requires more than pillows can offer.
References
1. Barakat-Johnson M, Lai M, Stephenson J, Buhr H, Campbell J, Dolton A, et al. Efficacy of a heel offloading boot in reducing heel pressure injuries in patients in Australian intensive care units: A single-blinded randomised controlled trial. *Intensive and Critical Care Nursing*. 2022 Jun;70:103205. DOI: 10.1016/j.iccn.2022.103205
2. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. 4th ed. EPUAP/NPIAP/PPPIA; 2025. Available from: https://www.internationalguideline.com
3. Gefen A. Why is the heel particularly vulnerable to pressure ulcers? *British Journal of Nursing*. 2017;26(Sup20):S62-S74. DOI: 10.12968/bjon.2017.26.Sup20.S62
4. Mak AFT, Zhang M, Tam EWC. Biomechanics of pressure ulcer in body tissues interacting with external forces during locomotion. *Annual Review of Biomedical Engineering*. 2010;12:29-53. DOI: 10.1146/annurev-bioeng-070909-105223
5. Kosiak M. Etiology and pathology of ischemic ulcers. *Archives of Physical Medicine and Rehabilitation*. 1959 Feb;40(2):62-69.
6. Greenwood C, Nixon J, Nelson EA, McGinnis E, Randell R. A realist evaluation of devices used for the prevention of heel pressure ulcers: An ethnographic study of clinical practice. *Applied Nursing Research*. 2024 Apr;76:151785. DOI: 10.1016/j.apnr.2024.151785
7. Bennett L, Kavner D, Lee BY, Trainor FS. Shear vs pressure as causative factors in skin blood flow occlusion. *Archives of Physical Medicine and Rehabilitation*. 1979 Jul;60(7):309-314.
8. Greenwood C, Nelson EA, Nixon J, Vargas-Palacios A, McGinnis E. Comparative effectiveness of heel-specific medical devices for the prevention of heel pressure ulcers: A systematic review. *Journal of Tissue Viability*. 2022;31(4):579-592. DOI: 10.1016/j.jtv.2022.09.002
9. Bennett G, Dealey C, Posnett J. The cost of pressure ulcers in the UK. *Age and Ageing*. 2004 May;33(3):230-235. DOI: 10.1093/ageing/afh072
10. Dealey C, Posnett J, Walker A. The cost of pressure ulcers in the United Kingdom. *Journal of Wound Care*. 2012 Jun;21(6):261-266. DOI: 10.12968/jowc.2012.21.6.261
11. National Institute for Health and Care Excellence (NICE). Pressure ulcers: prevention and management. Clinical guideline [CG179]. London: NICE; 2014 (updated 2019). Available from: https://www.nice.org.uk/guidance/cg179
12. Ulcer Solutions Inc. Heel Keeper vs Traditional Heel Elevating Off-Loading Boot for Pressure Injury Prevention/Treatment: A Preliminary Adherence Study. Ulcer Solutions Clinical Report; 2023. Available from: https://www.ulcersolutions.com