Why your NMES product probably doesn't work with denervated muscle.
It's not unusual for us to receive a call from a client with a spinal cord injury or a peripheral nerve injury who has been trying to use a handheld NMES (a form of Functional Electrical Stimulation) product and can't seem to produce a muscle contraction. The reason is likely because the muscle is denervated, and the NMES unit is unsuitable for that application. This article will explain why these units will not be suitable when denervated muscles are present, especially if it has been some time since the injury. We will also discover what can produce a restorative muscle contraction when denervation is present.
Electrical Stimulation and Action Potential
Functional Electrical Stimulation (FES) comes in many valuable forms in rehabilitation. The techniques tend to be safe, easy to apply, and effective, with decades of clinical use behind them. After injury or illness, FES can strengthen muscles, restore functional movement or even relax tight muscles when necessary. However, all techniques and products have indications, contraindications and basic limitations.
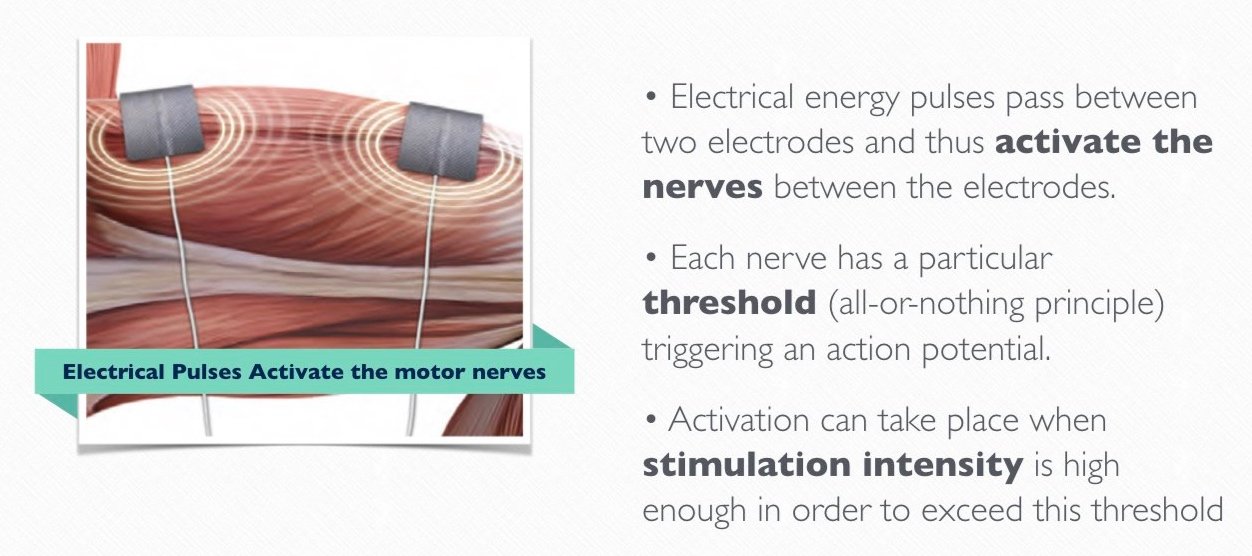
Practically all established clinical FES applications are based on direct excitation of the nerve structures, which indirectly activate muscles to produce a contraction. This is often referred to now as NMES (Neuro-muscular electrical stimulation). In this approach, a pair of gelled electrodes are placed on the belly of the muscle involved, and the FES unit generates the necessary and sufficient electrical energy to penetrate the skin and surface tissues, activate the nervous structures, and thereby generate muscle contraction.
The fundamental science of this approach has been described in many texts and is beyond the scope of this article. Still, we should understand that this approach fundamentally takes advantage of nerves having a ‘resting’ membrane potential.
The nerve membrane is always energetically charged due to the unequal flow of ions across it. The body uses energy to maintain this state, but the result is efficient. A nerve is always ready to 'fire' when it receives a suitable 'command'. The nerve transmits an 'action potential' or nerve impulse when received from the controlling nervous system or in rehabilitation from the FES unit.
When considering electrical stimulation, the only real difference with what happens in nature is that the action potential is ‘forced’ or somehow stimulated along the nerve's length. The electrical energy is the external stimulus that initiates the action potential within the nerve. Assuming that the energy is sufficiently large to overcome a threshold level, then the action potential that results from the electrical stimulation is identical to one that is initiated ‘naturally’ by the nervous system.
As we will describe in the section below, denervation results in the deterioration of the nerve structure within the muscle so that this mechanism can no longer be used to initiate a muscle contraction. There are other changes to the muscle tissue structure, but the detrimental changes to nerves are more rapid. Due to the absence of the neuromuscular junction and decomposition of motor units, muscular contractions can only be produced by depolarising the cellular membrane of each single muscle fibre rather than relying on the nerve structure.
In simple terms, to work with denervated muscle we must apply stimulation energy that directly affects the muscle fibres.
The electrical energy pattern produced by most NMES units is commonly in the form of repeated biphasic pulses controlled in voltage or current flow to produce the desired effects when the nerve structure is intact (i.e. trigger the action potential). It is usual to describe stimulation parameters such as pulse width, frequency and voltage or current to characterise the energy pattern used. Devices produced for sports or NMES medical applications are generally specified by regulatory authorities to limit the energy through the electrode/tissue interface to avoid skin burns. As we will see, the technical demands for electrical stimulation are completely different for the reactivation of denervated and especially denervated and degenerated muscles.
What is denervation anyway?
The complex response of muscle tissue to denervation is one of the most studied processes in muscle physiology and pathology. Muscle denervation is an adverse effect of sensory or motor nerve injury. Some of the most common causes are direct nerve damage, spinal cord injury, and various types of neuromuscular diseases. Denervation can occur due to any condition or injury affecting the nerves that supply the muscles. In these cases, nerves are effectively no longer connected to the muscles they once controlled.
Suppose the injury occurs at the level of the lumbar or sacral spinal cord or the conus medullaris (the lower end of the spinal cord). In that case, it can directly affect the Lower Motor Neurons (LMN) that exit the spinal cord at these levels and branch to the muscles they serve. These neurons innervate the muscles of the lower limbs and pelvic region. LMN injuries often result in flaccid paralysis, characterised by weak, floppy muscles, reduced or absent reflexes, muscle atrophy, and sometimes muscle twitches (fasciculations) in the early stages. This results in higher risk of pressure ulcers, poor circulation and a generally poor trophic situation.
As we learned above, this disconnection leaves muscles unresponsive to typical NMES treatments because the usual pathways for stimulation are disrupted, and the energy these units can deliver is insufficient.
Neurotrophic Theory
The denervated muscle has been studied for many decades, but the main leaps forward in understanding have depended on forming multidisciplinary teams drawing on the expertise of many different specialisations. At its publication, Ernest Gutmann’s book, “The Denervated Muscle” (Guttman, 1962), was a landmark effort and the first major consolidation of a large body of literature on muscle denervation. It laid out many important issues involving what was known as a neurotrophic theory in a manner that allowed them to be experimentally tested. The body of research at this time was primarily descriptive in nature and lacked the means to verify aspects of the theory.
The neurotrophic theory suggests that neurons (nerve cells) require specific neurotrophic factors for survival, development, and function. Neurotrophic theory is a complex field with ongoing discoveries. Research conducted since has demonstrated that muscle activity and not neurotrophic factors are primarily essential for the regulation of muscle fibre properties.
Is electrical stimulation of denervated muscle worthwhile?
By 1996, Eberstein asked whether electrical stimulation of denervated muscle was worthwhile. Secondly, the authors wanted to address the widespread belief that stimulation would prevent reinnervation.
They reported that electrical stimulation can be considered a useful procedure for preserving or restoring the normal properties of denervated muscles. However, stimulation can only be of benefit if an appropriate stimulation pattern is used. Because the muscle fibres needed to be stimulated, a different energy pattern was required compared with that used with NMES. It also, of course, required muscle fibre structures to be largely intact and capable of contracting. It was known that fibres would degrade following a denervation incident, but luckily, the fibre structures survive longer than once thought.
Numerous studies indicate that optimal results occur when the muscle activity evoked mirrors the stimulation pattern of a normal motor neuron. Commencing stimulation before one year of denervation has passed was reported to be crucial. They also stated that the best time to initiate stimulation is immediately post-nerve injury. While treatment beginning months after nerve injury can partly reverse the degenerative process, they believed that the delay between denervation onset and stimulation start diminishes the recovery potential. They also stated that stimulating denervated muscle does not effectively impede axon regeneration or reinnervation.
The initial discoveries and suggestions regarding the stimulation of denervated muscles were primarily based on animal studies. Eberstein recognised that many of these findings would also apply to human denervated muscles but required verification. In the late 1990s, exploring and verifying the most effective stimulation protocols for human denervated muscles was necessary.
Austria and the RISE Study
Meanwhile in Austria - In 1990 Dr. Helmut Kern achieved his Habilitation for M.D. with a thesis that has been published in German in the Oesterreichische Zeitschrift fuer Physikalische Medizin 1995; 5: Heft 1, Supplementum. and since in English.
This study with Functional Electrical Stimulation (FES) involving 16 paraplegic patients showed significant improvements after 8 months of specialist FES training. Muscle biopsies, CT scans, and perfusion tests indicated increased muscle diameter, perfusion, and enzyme levels. FES demonstrated fibre hypertrophy and structural benefits in denervated muscles. Recommendations included using specific currents for optimal muscle contractions and integrating FES into modern rehabilitation to prevent muscle degeneration. FES was found to improve metabolism, trophic changes, cardiovascular fitness, and muscle activation in paraplegic patients.
The work of Guttman inspired Helmut Kern and Ugo Carraro to rigorously investigate the value of electrical stimulation in rescuing denervated muscle. The strong leadership of Helmut Kern convinced Engineers in Vienna and myologists in Italy (Carraro’s team in Padua and Feliciano Protasi in Chieti) to go on to implement two pilot trials supported by the EU Project RISE. (European Project RISE: Use of electrical stimulation to restore standing in paraplegics with long-term denervated degenerated muscles). The first activity was a cross-sectional study followed by a longitudinal study demonstrating that a home-based Functional Electrical Stimulation (hbFES) strategy could recover muscle mass and permanently denervate human muscle functions. The RISE study succeeded in bringing this area to the attention of many clinicians. Although focused on cases of complete denervation, it encourages further exploration of the potential in cases when reinnervation might be expected.
Stimulation Parameters for Denervated Muscle
Until now, we have stated that the stimulation parameters typically used with NMES units will not generate contractions with denervated muscle. However, we did not state what will work, so let's compare typical stimulation parameters for the two situations.
For NMES, the following stimulation parameters are typical of those in good-quality products.
The pattern of stimulation - biphasic rectangular pulse trains
Frequency - 20 to 50 Hz
Pulse widths - 100 to 500 microseconds
Amplitude (current) - 10 to 130 mA
For lower motor neuron injury situations
The stimulation pattern - biphasic rectangular pulse trains modulated in surges; sometimes biphasic, triangular pulse trains are used.
Frequency - 0.5 to 20 Hz
Pulse Widths - 40 to 200 ms
Amplitude - up to 250 mA
We see that we generally use lower frequency pulses with much longer pulse widths and higher currents for denervation situations. These are necessary to excite the muscle fibres in these cases.
The protocols from the RISE study and developed since then are individually customised to encourage an initial restoration of muscle excitability via a "twitch" contraction. A "tetanic contraction" is introduced as soon as possible to restore tissue bulk and muscle quality.
The values used will vary from person to person, but as an example, impulse durations (pulse widths) of 120 to 150 ms or even longer are used to produce a twitch contraction. As training progresses, this impulse duration is gradually reduced to produce a tetanic contraction. Stimulation may be applied to the affected limbs for 3 or 4 sets of 3 to 5 minutes with a rest between sets. We advise users to work with stimulation at least 5 days per week.
With current levels potentially much higher than those used in NMES situations, attention should be paid to managing the current density at the skin-electrode interface. Gelled electrodes, such as those used in NMES, are unsuitable and cannot be used. We typically use either a wet sponge, carbon rubber electrode pair, or special safety electrodes with electrode gel.
Remember that the aim is not to excite the nerve structure but the muscle fibres. For this reason, the electrodes tend to be large and cover as much of the muscle of interest as possible. Electrodes must be held in intimate contact with the tissue to ensure that the energy field generated is even and effective.
It is often the case with NMES that individual muscles should be activated. However, when working with denervated muscle, we typically wish to activate a whole muscle group and are not trying to work with single muscles selectively. For example, when working with completely denervated thigh muscles, we understand that even the hamstring muscles will be activated beneficially. There may be cases when we use a triangular form of biphasic pulse to select a denervated muscle when it is close to muscles with preserved innervation.
The Schuhfried Den2x and RISE stimulator
Shortly after the publication of the RISE study, we were pleased to be able to work with the Den2x product from Dr. Schuhfried Medizintechnik GmbH in Vienna. This innovative 2 channel stimulator allowed us to replicate the stimulation parameters utilised in the RISE study and bring this technology to many home-based clients in the UK. This unit required a change in regulatory approval due to the currents generated potentially being up to 300 mA. In practice, we rarely needed to approach this level. The recent introduction of the two-channel RISE stimulator gave us a much nicer interface to see and change stimulation parameters at a glance. The maximum current has been reduced to 250 mA, which has been sufficient in our experience.
A new feature in this product is introducing the "impulse" test. We have always wanted a simple method of quantifying the extent of denervation. In cases of complete denervation, this has allowed us to monitor the progress of training.
We have produced a number of videos that show the use of this RISE unit in detail. Please contact us for details of these videos and to be advised of upcoming webinars on this topic area.
Articles
Gutmann E, ed: The Denervated Muscle. Publ. House of Czechoslovak Academy of Sciences, Prague, 1962, pp. 486.
Eberstein A, Eberstein S. Electrical stimulation of denervated muscle: is it worthwhile? Med Sci Sports Exerc. 1996 Dec;28(12):1463-9. doi: 10.1097/00005768-199612000-00004. PMID: 8970139.
Kern H. Habilitation Thesis Functional Electrical Stimulation on Paraplegic Patients. Eur J Trans Myol – Basic Appl Myol 2014; 24
Kern H, Carraro U, Adami N, Biral D, Hofer C, Forstner C, Mödlin M, Vogelauer M, Pond A, Boncompagni S, Paolini C, Mayr W, Protasi F, Zampieri S. Home-based functional electrical stimulation rescues permanently denervated muscles in paraplegic patients with complete lower motor neuron lesion. Neurorehabil Neural Repair. 2010 Oct;24(8):709-21. doi: 10.1177/1545968310366129. Epub 2010 May 11. PMID: 20460493.
https://www.sciencedirect.com/topics/nursing-and-health-professions/muscle-denervation